-
PDF
- Split View
-
Views
-
Cite
Cite
Laura DiChiacchio, Clint D Cappiello, Jose Greenspon, Extracorporeal cardiopulmonary resuscitation in a neonate after air embolism during insufflation for laparoscopic peritoneal dialysis catheter placement, Journal of Surgical Case Reports, Volume 2018, Issue 6, June 2018, rjy119, https://doi.org/10.1093/jscr/rjy119
Close - Share Icon Share
Abstract
Laparoscopy is increasingly utilized in neonatal surgery with safe and effective outcomes. Air embolism from insufflation for pneumoperitoneum is a rare but known risk of laparoscopy. Here we present a rare case of air embolism during insufflation for laparoscopic peritoneal dialysis catheter placement treated with extracorporeal cardiopulmonary resuscitation.
CLINICAL SUMMARY
Our patient was an ex-36 week and 5-day male infant previously managed at our fetal care center for bladder outlet obstruction with anhydamnios requiring cystocentesis, multiple amniocenteses with amnioinfusion and placements of both vesicoperitoneal and vesicoamniotic shunts. His mother developed preterm, premature rupture of membranes and his delivery was otherwise uncomplicated. On day of life one, the neonatal intensive care team placed an umbilical catheter for central venous access and he underwent cystoscopy, ablation of posterior urethral valves, wire-guided placement of bladder catheter, circumcision and removal of vesicoamniotic shunt by pediatric urology. Postoperatively, he remained oliguric and his creatinine continued to rise. On day of life 6 with continued worsening renal function, it was felt that renal replacement therapy needed to be initiated and the patient taken to the operating room for laparoscopic peritoneal dialysis catheter placement.
Upon arrival to the operating room, the patient’s umbilical vein catheter was used for induction and peripheral venous access was obtained by anesthesia. The umbilical catheter was prepped into the sterile field and removed with return of venous blood. Hemostasis was achieved using transmitted electrocautery. Dissection was performed bluntly with a clamp through the umbilical stump as lateral as possible to the entry point of the umbilical vein. The clamp entered easily without return of blood. A 3-mm blunt trocar was placed easily without resistance. There was again no return of blood. Insufflation was initiated and the scope was passed through the trocar. Immediately it was recognized that the scope was in a lined tubular structure not consistent with mucosa and not within the abdominal cavity proper. At this point, anesthesia notified the surgical team that there was sudden complete loss of end tidal carbon dioxide. The scope and trocar were removed and pneumoperitoneum promptly evacuated. However, almost simultaneously, the patient became profoundly bradycardic. A red rubber catheter was passed along the trocar tract and venous blood mixed with air was aspirated. The patient became pulseless and cardiopulmonary resuscitation (CPR) was initiated with pediatric advanced life support (PALS) protocol. Aspiration of the air embolism was attempted via the right internal jugular vein in Trendelenburg position (Durant maneuver). Venous blood and air were ultimately aspirated from this site under ultrasound guidance without improvement in hemodynamics.
At this point, the decision was made to proceed to ECPR. The right internal jugular vein and right carotid artery were accessed via direct cutdown and cannulated with 8Fr cannulas. Chest compressions were held and extracorporeal life support (ECLS) was initiated at 100 ml/kg. The patient converted to a sinus rhythm. An echocardiogram confirmed positioning of the cannulas and revealed persistent air in the left and right atria without evidence of pericardial effusion. At this point, the umbilicus was closed and the patient was transferred to the neonatal intensive care unit intubated and in critical condition with ongoing ECLS.
The patient was cooled for 24 h and required hemofiltration through the ECMO circuit for anuria. Approximately 12 h into his ECMO run, the patient developed pericardial tamponade demonstrated on echocardiography, likely secondary to chest compressions, requiring one round of CPR and placement of a percutaneous pericardial drain. Body X-ray (Fig. 1) demonstrated pericardial drain, arterial, and venous cannulae placement. A head ultrasound was obtained the following morning that demonstrated air in the lateral ventricles, Grade I intraventricular hemorrhage and a cerebellar infarct. His neurologic prognosis was deemed by neonatology and pediatric neurology to be exceedingly poor and his mother requested care to be withdrawn. The patient expired within minutes of withdrawal of ECLS. An autopsy was performed that revealed a laceration in the umbilical vein. Autopsy additionally demonstrated myocardial hemorrhage and pulmonary edema consistent with cardiogenic shock.
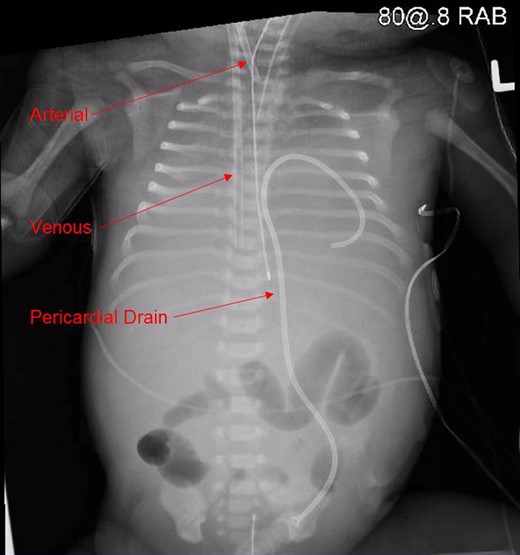
Body X-ray demonstrating pericardial drain, arterial and venous cannulae placement.
DISCUSSION
Laparoscopy in neonates is both common and safe. Air embolism from insufflation for pneumoperitoneum is exceedingly rare, with five prior reported cases in the literature. All of the reported cases describe a known or suspected umbilical vein laceration as the entry point for insufflation [1–4]. It is important to note that priming insufflation tubing with carbon dioxide, rather than initiating insufflation with nitrogen-rich room air, significantly reduces the likelihood of poor outcome in the case of venous gas embolism in the neonate [1]. Extracorporeal CPR (ECPR), when contrasted with conventional CPR provides better outcomes when considering both survival to discharge and neurologic recovery [5]. Here we present a case of gas embolism during insufflation for laparoscopic peritoneal dialysis catheter placement recovered with ECPR. Unfortunately, because future neurologic recovery was deemed unlikely, the family requested withdrawal of care. This is the first death due to air embolism from insufflation in a neonate that has been reported to our knowledge; it is also the first reported case utilizing ECPR for temporization of obstructive cardiogenic shock in a neonate secondary to air embolism.
Conflict of interest statement
None declared.



