-
PDF
- Split View
-
Views
-
Cite
Cite
Evan R Brownie, Robert W Thompson, Effort thrombosis of the subclavian artery as a consequence of a unique anomaly, Journal of Surgical Case Reports, Volume 2018, Issue 4, April 2018, rjy072, https://doi.org/10.1093/jscr/rjy072
Close - Share Icon Share
Abstract
Congenital anatomic anomalies and variations are frequent in the thoracic outlet and may be associated with clinical symptoms. Arterial thoracic outlet syndrome (TOS) is characterized by subclavian artery compression and vascular pathology, almost always in the presence of a bony abnormality. We describe here a patient with arterial thromboembolism following a fall on the outstretched arm, who was found to have subclavian artery stenosis and post-stenotic dilatation in the absence of a bony abnormality. Surgical exploration revealed a previously undescribed anomaly in which the subclavian artery passed through the costoclavicular space in front of the anterior scalene muscle, where it was subject to bony compression between the first rib and clavicle. Successful treatment was achieved by scalenectomy, first rib resection and interposition bypass graft reconstruction of the affected subclavian artery. This newly acknowledged anatomical variant adds to our understanding of the diverse factors that may contribute to development of TOS.
INTRODUCTION
Thoracic outlet syndrome (TOS) refers to a group of uncommon disorders arising from extrinsic compression of the neurovascular structures that serve the upper extremity [1]. Safe and effective treatment for the various forms of TOS requires that the surgeon be familiar with the complex neural, vascular, muscular and bony anatomy of this region, including the scalene triangle, the costoclavicular space and the subcoracoid (pectoralis minor) space [2]. In addition, the thoracic outlet surgeon must be aware of a wide spectrum of anatomical anomalies and variations that may be encountered, to ensure complete decompression and to avoid injury to vital structures [3–8].
The arterial form of TOS is characterized by focal subclavian artery compression accompanied by vascular pathology that may include stenosis, occlusion, aneurysmal dilatation, ulceration and/or thromboembolism, almost always in the presence of a bony abnormality [9]. We describe here a patient presenting with upper extremity arterial thromboembolism following a fall on the outstretched arm, who was found to have subclavian artery stenosis and post-stenotic dilatation in the absence of a bony abnormality. Surgical exploration revealed a previously undescribed anomaly of the subclavian artery making it subject to bony compression between the clavicle and first rib. The patient described in this report provided consent for publication.
CASE REPORT
An otherwise healthy 44-year-old female nurse presented with a painful left arm and hand, 2 weeks after she had fallen onto the outstretched left arm while hiking. She sought medical attention when she developed Raynaud’s phenomenon and was unable to feel pulses at the wrist, and clinical evaluation suggested thrombosis of the left brachial, radial and ulnar arteries. Contrast-enhanced computed tomography (Figs 1 and 2) and catheter-based arteriography (Fig. 3) confirmed the diagnosis and showed that while there was no cervical rib or other bony abnormality, there was focal stenosis of the left subclavian artery at the level of the first rib with mild post-stenotic dilatation. These findings indicated that the subclavian artery was the source of thromboembolism and the patient was successfully treated with catheter-based thrombolysis to resolve the acute obstruction. She was discharged on a direct oral anticoagulant but returned within several weeks after recurrence of symptoms. She was found to have rethrombosis and again underwent thrombolysis, followed by anticoagulation with an alternative agent, and was then referred to our specialized TOS center for surgical treatment.
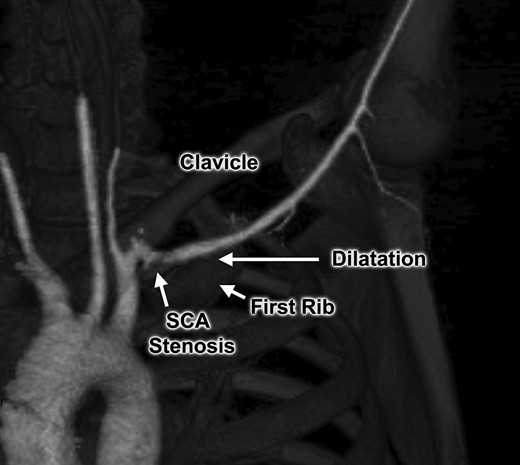
Computed tomography angiogram with 3D reconstruction, demonstrating focal left subclavian artery (SCA) stenosis and post-stenotic dilatation within the thoracic outlet.
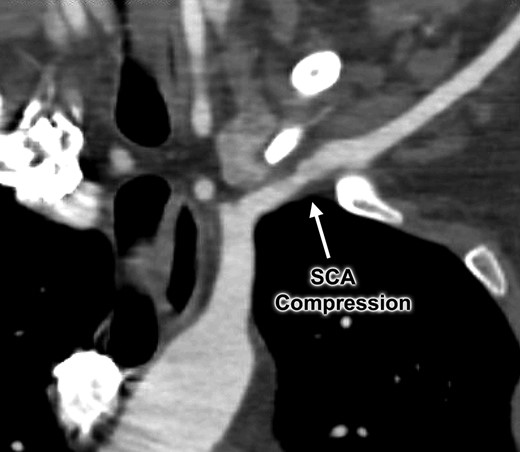
Computed tomography angiogram demonstrating focal area of left subclavian artery (SCA) compression between the first rib and clavicle.
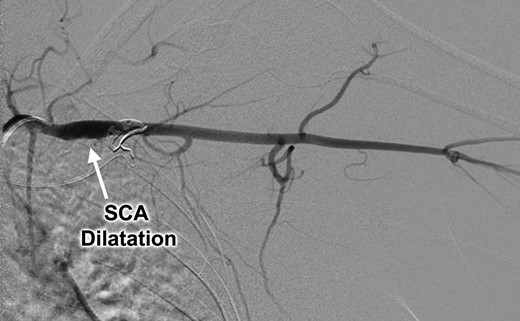
Catheter-based left subclavian arteriogram demonstrating post-stenotic aneurysmal dilatation of the subclavian artery (SCA).
Clinical evaluation revealed an absence of palpable pulses at the left wrist but adequate arterial circulation to the hand at rest, with brisk capillary refill in the fingers and no signs of digital embolism. Upper extremity strength, sensation and range of motion were normal and there were no signs of swelling, edema or cyanosis to suggest venous obstruction. The patient was brought to the operating room for thoracic outlet decompression using a left supraclavicular approach. After mobilizing and rotating the scalene fat pad on a lateral pedicle, the phrenic nerve was identified in its expected position on the surface of the anterior scalene muscle; however, the subclavian artery was not found within the scalene triangle adjacent to the brachial plexus, but in front of the anterior scalene muscle insertion on the first rib, in the costoclavicular space directly posterior to the phrenic nerve (Figs 4 and 5). Thoracic outlet decompression was performed with anterior and middle scalenectomy, brachial plexus neurolysis and first rib resection [10]. Direct inspection and intraoperative left upper extremity arteriography demonstrated post-stenotic dilatation of the subclavian artery and chronic occlusion of the brachial artery with abundant collaterals. The affected segment of the subclavian artery was resected and found to contain an ulcerated lesion with thrombus (Fig. 6), and the artery was reconstructed with a 6-mm diameter cryopreserved femoral artery interposition graft (Fig. 7). The patient was discharged on postoperative Day 3 taking a direct oral anticoagulant and she was clinically stable during subsequent follow-up.
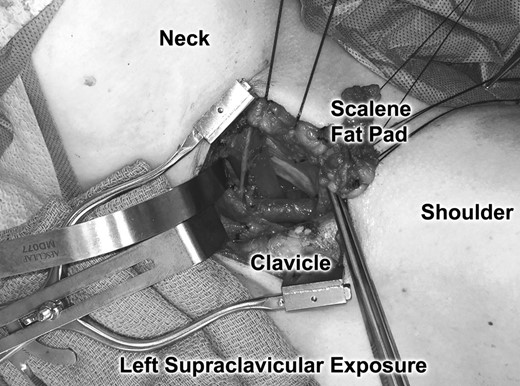
Operative photograph demonstrating initial exposure of the left supraclavicular space, with the scalene fat pad mobilized and rotated laterally. The subclavian artery was found in the costoclavicular space in front of the anterior scalene muscle.
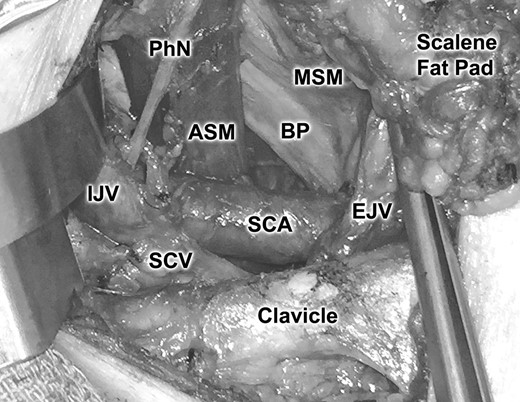
Close-up view of the subclavian artery and related structures. ASM, anterior scalene muscle; BP, brachial plexus; EJV, external jugular vein; IJV, internal jugular vein; PhN, phrenic nerve; MSM, middle scalene muscle; SCA, subclavian artery; SCV, subclavian vein.
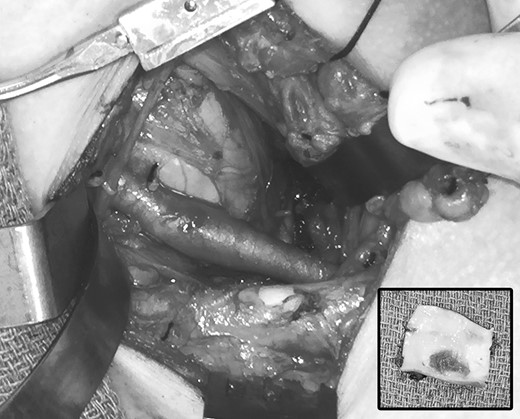
Operative photograph after thoracic outlet decompression, demonstrating area of post-stenotic dilatation in the left subclavian artery. Inset, excised segment of the affected left subclavian artery, demonstrating ulceration and thrombus on the luminal surface.

Operative view after reconstruction of the left subclavian artery with a cryopreserved femoral artery interposition bypass graft.
DISCUSSION
Anatomic variations have been frequently described within the scalene triangle and spaces of the thoracic outlet, both in the normal population and in patients with TOS [3–8]. These variations typically include bony anomalies (e.g. cervical ribs and hypoplastic first ribs), muscular variants (e.g. the scalene minimus muscle) and a spectrum of fibrofascial bands and ligaments. Such anomalies may predispose patients to the development of compressive neurovascular symptoms following trauma or mechanical stress, resulting in the clinical manifestations of TOS. Knowledge of these anatomical variations is particularly important to surgeons conducting operations for TOS, in order to ensure safe and thorough decompression.
In this report we describe a patient with a unique anomaly in which the subclavian artery passed through the costoclavicular space in front of the anterior scalene muscle, in the space usually reserved for the subclavian vein, rather than through the scalene triangle in association with the brachial plexus. We are unaware of any previous reports describing this anomaly and the senior author has not observed this anatomical variation in a clinical experience that exceeds 3000 operations for the various forms of TOS. It appears likely that the abnormal position and course of the subclavian artery in this patient was a predisposing factor in arterial compression and development of post-stenotic dilatation. Moreover, the path of the subclavian artery through the medial costoclavicular space, similar to the position of the subclavian vein, may have made the vessel more prone to injury during a fall on the outstretched arm, which in this case appeared to have precipitated the acute thromboembolic event. This clinical scenario is similar to that occurring when the subclavian vein is compressed between the medial first rib and clavicle during repetitive arm elevation, resulting in the clinical condition described as ‘effort thrombosis’ of the subclavian vein. The newly acknowledged anatomical variant observed in this patient, resulting in pathophysiologically similar ‘effort thrombosis’ of the subclavian artery, thereby adds to our understanding of the diverse factors that may contribute to different forms of TOS.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
Supported by the Thoracic Outlet Syndrome Research and Education Fund of the Foundation for Barnes-Jewish Hospital.
REFERENCES
- thromboembolism
- clavicle
- reconstructive surgical procedures
- subclavian artery
- subclavian steal syndrome
- thoracic outlet syndrome
- tissue transplants
- arm
- pathology
- paget-schroetter syndrome
- bypass
- thoracic outlet
- scalenectomy
- excision of first rib
- groove for costoclavicular ligament
- compression
- scalenus anterior muscle
- rib, first
- exploratory surgery
- poststenotic dilatation



