-
PDF
- Split View
-
Views
-
Cite
Cite
Richard H McCarroll, Leslie J Moore, Transanal minimally invasive surgery for resection of retrorectal cyst, Journal of Surgical Case Reports, Volume 2018, Issue 2, February 2018, rjy021, https://doi.org/10.1093/jscr/rjy021
Close - Share Icon Share
Abstract
Tailgut cysts are benign retrorectal embryological remnants, often found incidentally or when evaluating a patient for pelvic symptoms. Transanal minimally invasive surgery (TAMIS) offers patients a low morbidity surgical approach for resection of a variety of low rectal lesions. This is a case report of resection of a tailgut cyst using TAMIS, including images and description of the steps of the procedure.
INTRODUCTION
Tailgut cysts are rare presacral embryologic remnants, located in the retrorectus space, and are often found incidentally. There is a 3:1 female predominance. Though usually asymptomatic, retrorectal lesions may cause symptoms of pain with defecation, pain in the deep pelvis or lower back, a sensation of fullness, bleeding and rarely urinary symptoms. When symptomatic, these lesions are more concerning for malignancy. The majority of retrorectal cysts are benign, but they do have the potential for malignant transformation, and therefore should be resected when found.
Traditionally, these have been resected using a posterior parasacrococcygeal approach. More extensive lesions may require an abdominal approach, or a combined abdominal and posterior approach. With the advent of transanal minimally invasive surgery (TAMIS), there is potential for a low morbidity, well-tolerated approach to resection. This is able to be accomplished using standard laparoscopic equipment, with transanal access. These considerations make TAMIS an appealing modality for resection of clinically benign retrorectal cysts.
CASE REPORT
This is a case report describing the resection of a presacral cyst in a 23-year-old male patient. The cyst was discovered incidentally on CT scan of the abdomen and pelvis for evaluation of acute appendicitis (Fig. 1). The patient denied pain, bleeding, or change in bowel habits. He had no neurologic changes. A follow-up MRI was also performed (Fig. 2), and imaging was consistent with a congenital retrorectal cyst, with a tailgut cyst being favored. There was no evidence of bony involvement or invasion of other structures (Figs 1 and 2).
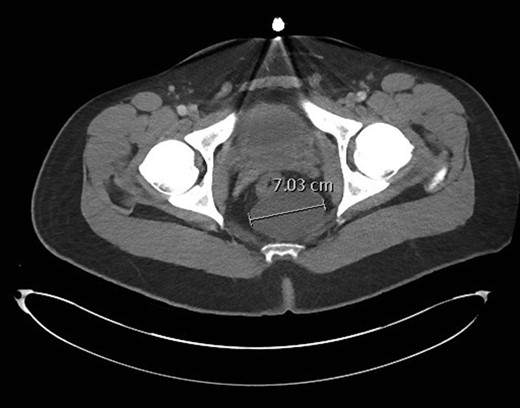
CT pelvis image demonstrating a 7.0 cm retrorectal cyst. The rectum is noted anterior to the cyst, and just to the right of midline.
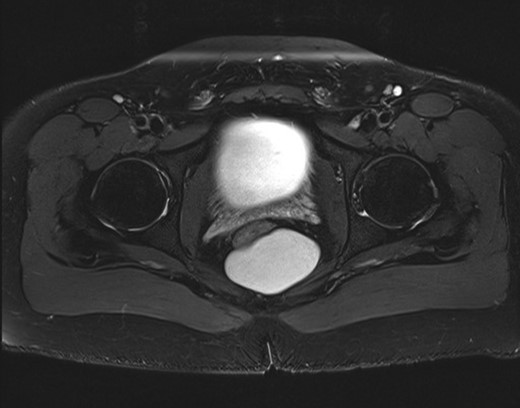
MRI pelvis demonstrating the retrorectal cysts, again with the rectum anterior and just to the right of midline.
The lesion showed no radiographic signs of malignancy, and was felt to be amenable to TAMIS resection. Preoperative preparation was done with a full mechanical and oral antibiotic bowel preparation. Preoperative parenteral antibiotics were administered. Under general anesthesia, the patient was placed in lithotomy position, and the perianal region was anesthetized prior to placement of a GelPOINT Path Transanal Access Platform (Applied Medical, Rancho Santa Margarita). The rectum was then insufflated.
After insufflation, the contour of the retrorectal cyst could be seen distorting the posterior wall of the rectum. Using an Harmonic Scalpel (Ethicon, Johnson and Johnson), a longitudinal incision was made through the posterior midline of the rectal wall, overlying the presacral cyst (Fig. 3) in doing so, the avascular plane surrounding the cyst was able to be exposed.
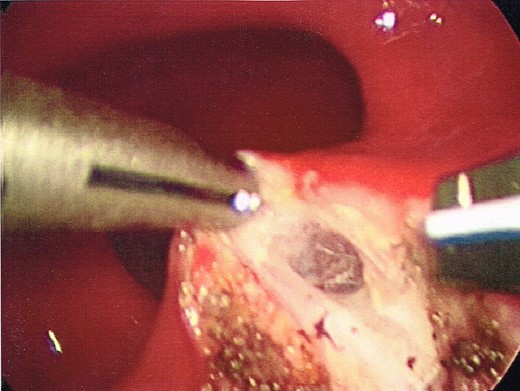
Opening of the posterior wall of the rectum, into the posterior perirectal space.
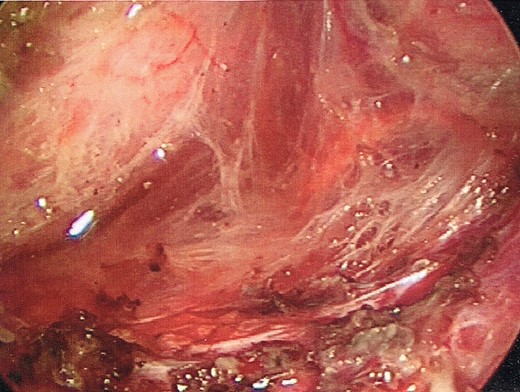
Once the dissection plane was entered, insufflation of the perirectal extraperitoneal space allowed for excellent exposure for a combination of blunt and Harmonic Scalpel dissection (Figs 4 and 5).
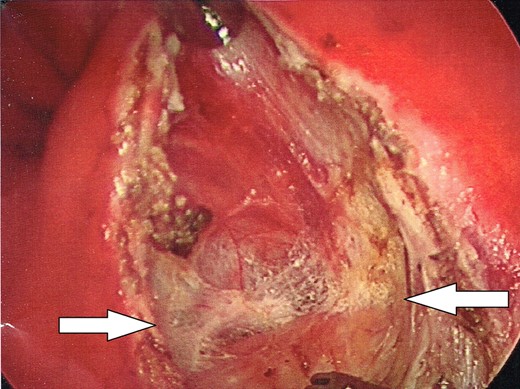
Enlargement of the proctotomy. The plane of dissection is visible (indicated by arrows), with the dome of the cyst seen at the bottom of the image.
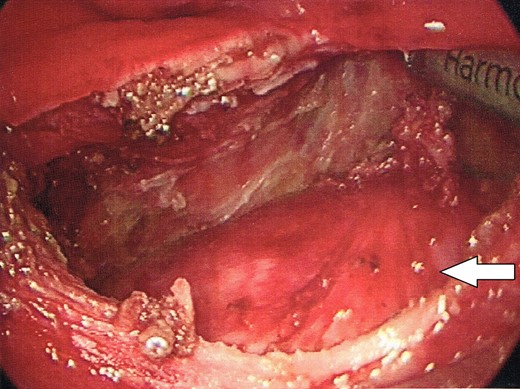
The dome of the cyst is visible at the bottom of the image (indicated by arrow), with a dissection plane visualized above.
The cyst was completely liberated from all attachments using TAMIS, with the exception of the caudal extent. The caudal extent of the cyst was unable to be adequately visualized with the TAMIS platform. Therefore, the transanal port was removed, and the resection of the distal extent of the cyst was completed transanally. The mass was then extracted transanally (Fig. 6).
The proctotomy was closed in a single layer with interrupted absorbable sutures. Following the procedure, the patient was discharged home. Final histology showed a benign keratinizing cyst. His postoperative course was uneventful.
DISCUSSION
Retrorectal cysts can lead to symptoms, and rarely harbor malignancy. When identified, these masses should be surgically excised. TAMIS allows for a minimally invasive approach to resection of tailgut cysts, and should be considered as an alternative to a posterior parasacrococcygeal approach, particularly for clinically benign lesions. Potential benefits of a TAMIS approach include minimal discomfort, decreased risk for sacral neurologic injury, excellent exposure and visualization of the cephalad extent of the cyst, and no visible scar. In addition, as no rectal wall is excised, closure of the proctotomy is able to be accomplished without tension or ischemia. In sum, TAMIS allows for a minimally invasive approach, with complete resection, decreased morbidity, and faster recovery and return to full activity.
Conflict of Interest Statement
None to disclose.



