-
PDF
- Split View
-
Views
-
Cite
Cite
Prateush Singh, Yehudit Bauernfreund, Pallavi Arya, Esha Singh, Justin Shute, Primary hyperparathyroidism presenting as acute psychosis secondary to hypercalcaemia requiring curative parathyroidectomy, Journal of Surgical Case Reports, Volume 2018, Issue 2, February 2018, rjy023, https://doi.org/10.1093/jscr/rjy023
Close - Share Icon Share
Abstract
Primary hyperparathyroidism (PHPT) can cause hypercalcaemia secondary to a pathologically high secretion of parathyroid hormone. Rarely this can first manifest as acute psychosis. It is imperative to exclude organic causes of psychosis before labelling the psychosis as primarily psychological. If hypercalcaemia is revealed, investigation is required to elucidate the underlying cause whilst instigating treatment to lower serum calcium levels. If PHPT is the underlying pathology, subsequent treatment involves surgical exploration and resection of the parathyroid adenoma or hyperplasia.
INTRODUCTION
Hypercalcaemia often presents with subtle clinical symptoms such as polyuria, polydipsia, weakness, irritability, abdominal pain and nausea. This vague clinical picture can delay accurate diagnosis until more significant complications arise such as acute pancreatitis, fractures and arrhythmias. Rarely, hypercalcaemia can manifest as acute psychosis.
We report the case of acute psychosis secondary to hypercalcaemia caused by primary hyperparathyroidism (PHPT) and its subsequent management with parathyroidectomy.
CASE REPORT
Our patient is a middle-aged Afro-Caribbean lady who was seen by the liaison psychiatry team after experiencing intimidating third-person auditory hallucinations, paranoid delusions, confusion, low mood and amnesia for 2 weeks. She was sleeping poorly and had reduced appetite. A collateral history from her daughter revealed that she had been laughing to herself, wandering without orientation and not attending work. There was no history of alcohol or drug consumption or smoking, and no pertinent family history.
She was orientated in time, place and person and her mental state examination revealed a well-kempt lady who maintained eye contact and spoke coherently.
On initial presentation, a psychiatric assessment was done but her serum calcium levels were not checked. She was started on an antidepressant (sertraline 50 mg) and an antipsychotic (olanzapine 10 mg) and discharged. She attended hospital two weeks later for worsening polyuria, polydipsia, anxiety and confusion. Investigations revealed raised levels of serum calcium (3.0 mmol/l), raised parathyroid hormone (PTH) (14 ng/l), low vitamin D (8 nmol/l), low serum phosphate (0.6 mmol/l) and a small left sided neck lump. Thyroid function tests, chest X-ray, CT-head and MRI brain were all normal.
From these results PHPT was suspected and the hypercalcaemia treated with intravenous fluids and a pamidronate infusion. Calcium levels normalized over the next few days along with her psychiatric symptoms suggesting a causative relationship. An ultrasound neck revealed an 11 mm lesion with echogenicity and internal vascularity, likely to be an atypical parathyroid adenoma (Fig. 1). A Sestamibi scintigraphy scan was inconclusive in correlating with the ultrasound or clinical impression, however, evidence was sufficient to warrant surgical exploration with removal of the adenoma as a definitive treatment for the PHPT and psychosis.
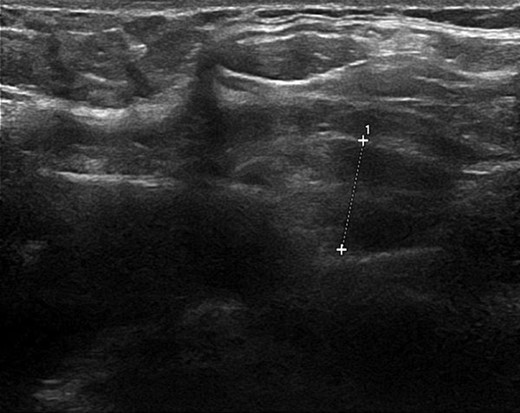
Ultrasound neck image illustrating the parathyroid adenoma measuring 11 mm with echogenicity and internal vasculature.
DISCUSSION
Psychosis may be the first manifestation of endocrine abnormalities such as Cushing’s syndrome [1], hyperthyroidism [2], hypothyroidism [3] and rarely PHPT [4].
A direct mechanism between hypercalcaemia and psychosis has not yet been elucidated. Calcium is known to have a role in determining monoamine metabolism in the central nervous system through modulation of dopaminergic and cholinergic metabolism and the release of neurotransmitters at synaptic junctions. Increased serum calcium has been observed during catatonic episodes in Schizophrenia patients [5]. Evidence for a correlation between severity of psychosis and degree of hypercalcaemia is inconclusive.
Hypercalcaemia has a multitude of causes including bone metastases, myeloma, a paraneoplastic response to PTH-related peptide from squamous cell carcinomas; iatrogenic complications from thiazides, vitamin A or D toxicity; inherited conditions including infantile hypercalcaemia and FHH; granulomatous diseases including sarcoidosis; neuroendocrine syndromes including multiple endocrine neoplasia, hyper or hypothyroidism, and hyperparathyroidism.
PTH is normally secreted from the parathyroid glands in response to low serum calcium levels; it acts on the kidneys and bone to increase serum calcium levels, and enhances the effects of vitamin D. It increases renal calcium reabsorption in the ascending loop of Henlé, distal tubule and collecting tubule, and increases phosphate excretion in the proximal tubule. PTH acts on bone by stimulating osteoclasts directly and indirectly via osteoblastic cytokines to pump calcium from bone fluid into extracellular fluid. PTH also increases conversion of 25-hydroxychloecalciferol to the more active 1,25-dihydroxycholecalciferol via the 1-hydroxylase enzyme in renal proximal tubules, thereby increasing calcium and phosphate absorption from the kidneys and alimentary canal.
Negative feedback is integrated into this system through inhibition of PTH secretion by high serum calcium levels acting directly on the parathyroid gland, thereby maintaining calcium levels within the normal range. In PHPT, PTH is autonomously secreted independently of this negative feedback, resulting in high PTH and calcium levels, and often low phosphate and vitamin D levels.
Up to 30% of cases of hypercalcaemia in PHPT are asymptomatic at presentation [6] with detection usually from coincidental blood tests. Clues in the history relating to symptomatic hypercalcaemia should prompt a full neck examination for parathyroid gland masses. Investigations should include an ECG which may reveal a shortened QT interval, J-waves or even ventricular arrhythmias. Blood tests may demonstrate high calcium, high PTH, low phosphate and low vitamin D levels indicating primary or tertiary hyperparathyroidism. Urea and electrolyte tests may indicate if the patient has chronic kidney disease which can result in tertiary hyperparathyroidism. Urinalysis may reveal calciuresis and if urine calcium levels are low, Familal hypocalciuric hypercalcaemia (FHH) may be suspected.
Neck ultrasound is the first line imaging modality and can illustrate abnormal masses. PHPT is caused by adenomas in 85% of cases, hyperplasia in 15% and carcinoma in under 1% of cases [7]. Ultrasound can help to differentiate the cause through assessing location, shape, echogenicity and vascularity.
Further imaging involves Sestamibi scintigraphy wherein the radionucleotide is more rapidly absorbed by hyperfunctioning parathyroid tissue than normal tissue allowing localization with a gamma camera. However, evidence suggests that Sestamibi scans are unreliable for small adenomas or multiglandular disease, with false negative rates of 22% and overall sensitivity 77% [8].
In the acute setting hypercalcaemia is treated with intravenous fluids, loop diuretics and bisphosphonates. Haemodialysis may be used when patients are unable to tolerate high volume hydration or with refractory hypercalcaemia [9]. The definitive treatment is surgical excision of the parathyroid adenoma. Pre-surgical localization imaging and hand-held intraoperative gamma probes allow for minimally invasive parathyroidectomy. Intraoperative PTH assays prior to and after adenoma excision with a decrease of >50% at 10 min post excision indicates successful resection, otherwise another adenoma or hyperplasia may be present, necessitating further exploration [10].
Acute psychosis is a rare manifestation of hypercalcaemia. We suggest investigation and exclusion of organic causes of psychosis before commencing psychiatric medication, as per the ICD-10 criteria, and where hyperparathyroidism is causative, only surgical excision is curative.
CONFLICT OF INTEREST STATEMENT
None.
FUNDING
None.
INFORMED CONSENT
Informed consent received from the patient for the production of this manuscript and the use of any accompanying images. Consent is available for review if required.
AUTHOR'S CONTRIBUTION
All authors contributed equally to the production of this article.
PRESENTATION
This article was presented as an international oral presentation at the European Society of Surgical Research, July 2017, Amsterdam, Netherlands.



