-
PDF
- Split View
-
Views
-
Cite
Cite
Ploutarchos Karydakis, Andreas Mitsios, Dimitrios Giakoumettis, Elias Antoniades, Aikaterini Karagianni, George Sfakianos, Marios Themistocleous, Primitive synovial sarcoma of suboccipital region in child, Journal of Surgical Case Reports, Volume 2018, Issue 10, October 2018, rjy286, https://doi.org/10.1093/jscr/rjy286
Close - Share Icon Share
Abstract
Synovial sarcoma (SS) most commonly affects the lower limbs of males in the third to fifth decades of life, with masses of the head and neck accounting for 3–10% of all cases, mainly as a metastatic lesion. The lack of specific symptoms and radiological features in addition to the diversity of their microscopic aspects may cause confusion in the diagnosis; hence, knowledge of the unusual locations of SSs is very important. The immunohistochemistry, and more recently the cytogenetic studies, contribute to the differential diagnosis. We report the case of a 12-year-old girl with a rare primary SS in the suboccipital region, which underwent complete surgical resection.
INTRODUCTION
Synovial sarcoma (SS) most commonly affects males in the third to fifth decades of life. It is the most common sarcoma of the foot, while only 3–10% of all SSs affect the head and neck mainly as metastatic lesions. We report the case of a 12-year-old girl with a rare primary SS in the suboccipital region, which underwent complete surgical resection.
CASE REPORT
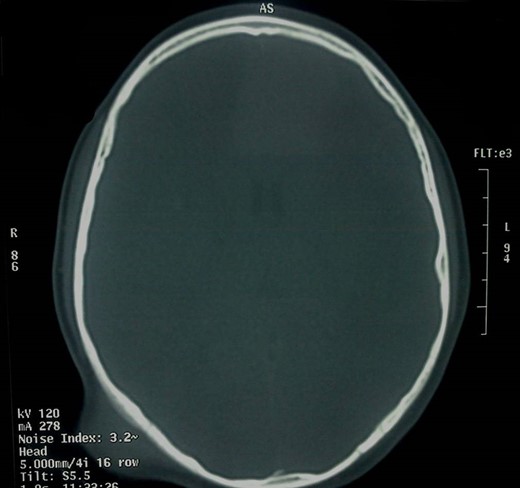
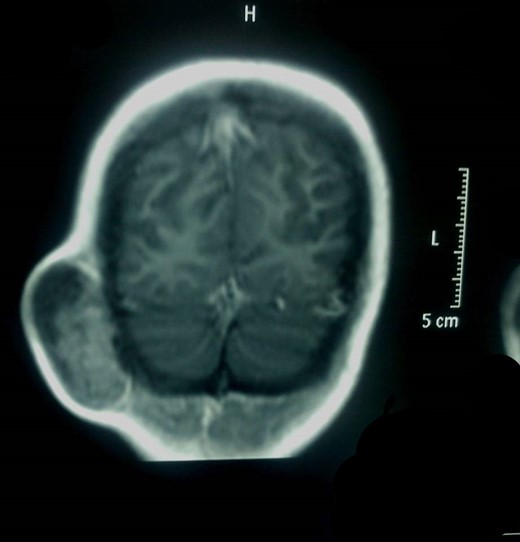
Α 12-year-old girl presented to us with a painless tumefaction on the right suboccipital region evolving for 5 months. Clinical examination did not reveal any other important symptoms or signs. Various explorations carried out, in particular, X-rays (Fig. 1), CT scan with intravenous contrast medium (Figs 2 and 3) and imagery by magnetic resonance with intravenous paramagnetic contrast.

Head profile X-ray. Bone thinning (white arrow) caused by the mass (red arrow).

MRI showed an encapsulated spindle formation in the region of the soft tissues of the right suboccipital region (Fig. 4). It was primarily located in the subcutaneous tissues, with a broad attachment to the outer table of the diploe, which appears to be thinned. It had mainly intermediate signal on T1W and T2W images, combined with some areas of high signal on T2 and low signal on T1. After the intravenous injection of the contrast, it showed inhomogeneous uptake.
The CT scan showed that there was only thinning of the bone without erosion or intracranial extension of the mass. There were no signs of calcification, and there was a mild and inhomogeneous uptake of the contrast.
The laboratory results did not show any specific features and the level of alkaline phosphatase was slightly elevated.
After consultation with our radiologists and oncologists, the girl was scheduled for tumor resection. In the operating room, she was placed in left lateral position, and we made a longitudinal incision over the lesion. We recognized a well-circumscribed mass, with hard consistency, which we exposed and excised en bloc, with a combination of blunt and sharp dissection. The bone underneath the lesion was eroded. When we excised the mass, it was found to be fibrous and viscous. The patient recovered well after the surgery and was discharged a few days later.
DISCUSSION
SS most commonly affects adults in the third to fifth decades of life. They represent 6–10% of all soft tissue sarcomas [1]. Only 3–10% of SSs found in the head and neck [2], mainly as a secondary lesion. Males are affected twice as often as females. The most common presentation is that of a painless mass, as described in our case; various associated symptoms may be present, depending on the location of the tumor. SSs do not arise from the synovial tissue; rather, they originate from pluripotential mesenchymal cells, and they rarely occur within joint spaces. They arise de novo from mesenchymal tissue, which differentiates sufficiently to have the histological appearance of synovium. The gross pathologic appearance is that of a white or grey mass, with a consistency that varies from firm, calcified or fibrous to soft, cystic or mucoid. Mesenchymal cells differentiate into two components: an epithelial-like cell layer and a connective-tissue layer of spindle-shaped cells.
The majority (80–95%) of tumors are reported in the extremities, with two-thirds being located in the lower limbs [3]. Other sites of origin, although rare, include the head and neck. The tumors are encapsulated and frequently in contact with bone. Because there are often few anatomical barriers, malignant spread to surrounding nerves and vasculature is common.
The unusual locations of the primitive SS must be known because the diversity of their microscopic aspects may cause confusion in the diagnosis. The immunohistochemistry, and more recently the cytogenetic studies, help to solve these problems of differential diagnosis. The differential diagnosis of poorly differentiated SS has to be done from small round blue tumors and spindle sarcomas. Ewing Sarcoma and Primitive NeuroEctodermal Tumor have as typical cytogenetic feature the translocation (11,22) while SS is characterized by SYT/SSX1 and SYT/SSX2 translocation. Additionally, rhabdomyosarcomas are characterized by the positivity for alveolar desmin, MyoD1, Myogenin. They are also characterized by the translocation (1, 13) and (2, 13) [4].
The prognosis varies, with the outcome of patients with non-extremity SS in general worse than that of patients with limb tumors but it appears to be relatively good for those patients whose tumor size is <5 cm, contains fewer than 10 mitoses/10HPF, and is devoid of a poorly differentiated component [5, 6]. The 5 years EFS and OS were 62.8 and 6.9%, respectively [7].
CONFLICT OF INTEREST STATEMENT
None declared.



