-
PDF
- Split View
-
Views
-
Cite
Cite
Ngoc-Bao Le, Nicole Rich, Ryan C Johnson, Laurence F Yee, Segmental intestinal dilatation associated with ileal gastric heterotopia in a young woman, Journal of Surgical Case Reports, Volume 2018, Issue 10, October 2018, rjy287, https://doi.org/10.1093/jscr/rjy287
Close - Share Icon Share
Abstract
Segmental intestinal dilatation (SID) is a rare gastrointestinal disorder characterized by marked bowel dilatation and can result in signs of intestinal obstruction, abdominal pain and gastrointestinal bleeding. SID is seen most commonly in pediatric patients, with most cases being reported in neonates and infants. Definitive treatment is resection of the dilated segment of bowel with primary anastomosis. This article describes a rare case of SID in an adult patient—a 26-year-old female who presented with chronic abdominal pain. The patient experienced complete resolution of symptoms following surgical resection.
INTRODUCTION
Segmental intestinal dilatation (SID) is a rare gastrointestinal (GI) disorder originally described by Swenson and Rathauser [1] in which there is a segment of marked bowel dilatation of up to 3- to 4-fold increase in size, flanked by normal-caliber bowel. SID was originally described in the colon, but has subsequently been reported in the small bowel, typically the ileum. Various associations exist, including Meckel’s diverticulum and omphalocele. Heterotopic rests of tissue have also been reported within the abnormal segment, including tissue with gastric, lung, pancreatic and esophageal histology [2]. Most cases of SID have been reported in neonates and infants [3]. Patients may present with signs of intestinal obstruction, abdominal pain, GI bleeding, anemia and/or failure to thrive [4]. Literature reporting SID occurring in adults remains extremely sparse. We present a case of a 26-year-old woman who presented with chronic abdominal pain, was found to have SID upon laparoscopy, and was successfully treated with bowel resection. Pathology review of the dilated small bowel segment revealed a 7 cm gastric heterotopic rest.
CASE REPORT
A 26-year-old woman with a history of omphalocele status post repair as a neonate presented to the emergency department (ED) for evaluation of recurrent severe abdominal pain. The abdominal pain was crampy, burning, periumbilical and associated with anorexia, bloating and constipation, mildly improved with induced vomiting. The patient experienced similar symptoms 1 year prior and underwent upper and lower endoscopy, gastric emptying study, and an abdominal ultrasound, all unremarkable. On presentation to the ED, her vital signs and laboratory results were all within normal limits. Conventional CT scan and CT enterography demonstrated a focally dilated segment of small bowel with normal afferent and efferent bowel on either side. Although imaging revealed no evidence of bowel obstruction or mass, diagnostic laparoscopy was performed due to her persistent symptoms. At laparoscopy, a 20 cm segment of abnormally dilated small bowel was identified in the mid ileum with a maximum width of 7 cm, bordered by normal-caliber small bowel (Fig. 1). The dilated segment was resected and an ileo-ileal anastomosis was performed. The resected segment was found to contain a 7 × 4.5 cm2 discrete island of abnormal appearing mucosa with rugal folding (Fig. 2). Histology revealed that this area consisted of heterotopic gastric glandular and foveolar epithelium with no abnormalities identified within the neuronal plexus proximal or distal to this mass (Figs 3 and 4). The patient had an uneventful recovery and was discharged home on postoperative day three. At 6-month follow-up, she reported no recurrence of her symptoms.
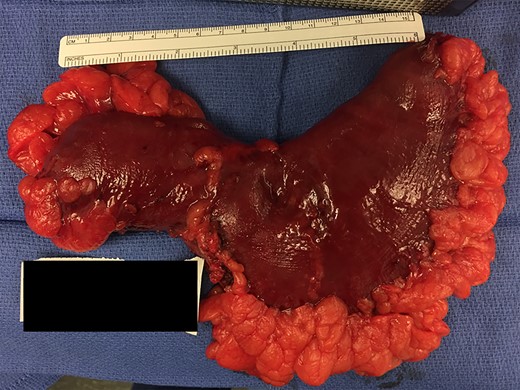

Resected specimen containing a 7 × 4.5 cm2 discrete island of abnormal appearing mucosa with rugal folding, later found to have histological characteristics consistent with heterotopic gastric tissue.
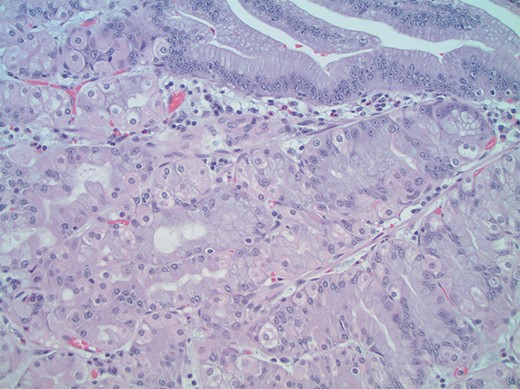
High-power magnification (×400) views of the mass show a mixture of gastric foveolar (top right) and fundic glandular epithelium including parietal and chief cells consistent with true gastric heterotopia.
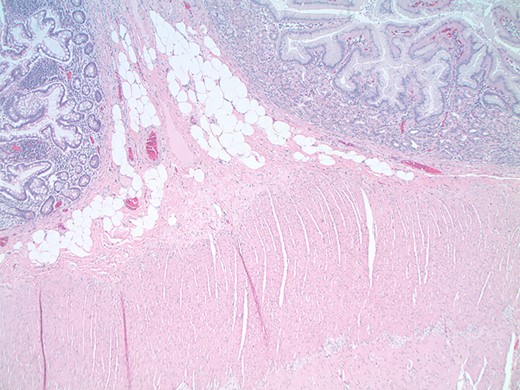
Low-power magnification (×40) views of the interface between the gastric heterotopia (right) and the small intestinal epithelium (left). Note that the muscularis propria (bottom) contains an intact neuronal plexus between the muscular layers.
DISCUSSION
The diagnostic criteria for SID were established by Swenson and Rathauser in 1959 and include:
Limited bowel dilatation with a 3- to 4-fold increase in size.
Abrupt transition between dilated and normal bowel.
No intrinsic or extrinsic barrier distal to the dilatation.
Clinical picture of intestinal occlusion or subocclusion.
Normal neuronal plexus.
Complete recovery after resection of the affected segment.
The etiology of SID remains poorly understood, but both pediatric and adult cases are thought to result from congenital processes [5]. One proposed mechanism suggests that the dilatation results from sustained compression of a segment of bowel at two ends by transient embryological structures such as vitelline vessels and omphaloenteric bands [2, 3]. Other theories involve intestinal dysgenesis resulting from impaired separation of the notochord from the endoderm and intestinal neuromuscular system disruption caused by ectopic tissue [6].
SID may be detected on plain radiographs, CT scans and barium enema studies. The classic appearance on plain radiograph is a sharply demarcated area of bowel dilatation with or without accompanying air-fluid levels [7]. Similarly, CT scans can demonstrate a segment of dilated bowel which may be found to contain oral contrast and fecal matter [8]. Barium enema may additionally reveal concomitant ulceration and absent valvulae conniventes [5]. Definitive treatment is resection of the dilated segment with primary anastomosis. Long-term prognosis is excellent [1].
Reported cases of SID in adults are extremely rare and our case is unique in several aspects. With regards to patient age, ~45% of reported cases have occurred in infants <4 weeks old, with up to half of these cases diagnosed within the first day of life [3, 9]. In a study of nine adult cases by Javors et al. [5], the mean age was 52 years. Our patient presentation at 26 years distinguishes this case from the literature on pediatric patients and demonstrates that adult cases can manifest even earlier than previously reported.
This case also highlights presenting symptoms that are less commonly seen in adult cases. Javors et al. [5] found that GI bleeding was the most common symptom in adults (77%) and that abdominal pain, signs of obstruction or both were reported in less than half of their patient cohort (44%). The GI bleeding often results from ulceration that occurs in the mucosa of the dilated segment or from heterotopic gastric mucosa. Our patient notably lacked signs of GI bleeding or anemia despite the heterotopic gastric mucosa identified in her specimen. Instead, it is presumed that the gastric secretions from the heterotopic tissue led to chronic irritation of the bowel and recurrent episodes of abdominal pain. The physical dilatation of the intestine itself was unlikely the primary cause of the pain, especially with the absence of any signs of obstruction or ischemia.
The relationship between SID and omphalocele has been described previously. Our literature review revealed only 17 reported cases of omphalocele associated with SID. In the majority of these cases, SID was found during omphalocele repair at birth [10]. However, in a few cases, such as in our patient, this GI disorder remained undiagnosed until symptoms manifested later in life.
In summary, SID is a rare cause of abdominal pain and GI bleeding in adults. Laboratory tests may reveal anemia and imaging studies can provide valuable information regarding the location of the structural defect. The majority of cases are treated successfully with resection of the dilated segment of bowel. In the case of our patient, the diagnosis of SID was not suspected until the time of laparoscopy. The patient has done extremely well following definitive resection.
ACKNOWLEDGEMENTS
None.
CONFLICT OF INTEREST STATEMENT
None.
FUNDING
None.



