-
PDF
- Split View
-
Views
-
Cite
Cite
Alexandra M. Limmer, Hoey C. Koh, Andrew Gilmore, Stricturoplasty—a bowel-sparing option for long segment small bowel Crohn's disease, Journal of Surgical Case Reports, Volume 2017, Issue 8, August 2017, rjx163, https://doi.org/10.1093/jscr/rjx163
Close - Share Icon Share
Abstract
Stricturoplasty is a surgical option for management of severe stricturing Crohn's disease of the small bowel. It avoids the need for small bowel resection and the associated metabolic complications. This report contrasts the indications and technical aspects of two different stricturoplasty techniques. Case 1 describes an extensive Michelassi (side-to-side isoperistaltic) stricturoplasty performed for a 100 cm segment of diseased small bowel in a 45-year-old patient. Case 2 describes the performance of 12 Heineke-Mikulicz stricturoplasties in a 23-year-old patient with multiple short fibrotic strictures.
INTRODUCTION
Small bowel strictures occur in 25% of patients with Crohn's disease [1]. Surgery is indicated for patients with obstructive symptoms despite optimal medical and/or endoscopic management [1]. Surgical options for strictures include resection, bypass or stricturoplasty [1].
Stricturoplasty was originally described in 1886 for management of pyloric strictures and was first utilized in Crohn's disease in 1982 [2, 3]. Stricturoplasty avoids the risk of short bowel syndrome associated with extensive resection [4]. It should be considered in patients with fibrotic strictures, especially those with multiple or long strictured segments or previous small bowel resection [5]. Contraindications include active inflammation, complications of Crohn's disease (including phlegmon, fistulae or perforation), suspected carcinoma and likely tension on the closure of the stricturoplasty [4, 5].
The following cases contrast two different stricturoplasty techniques for management of long segment stricturing Crohn's disease.
CASE REPORT
Case 1: A 45-year-old gentleman with a twenty year history of Crohn's disease and previous resection of 6 cm of ileum suffered from recurrent symptoms of small bowel obstruction. Magnetic resonance enterography showed multiple long strictures in the distal small bowel. The patient was forewarned of the possibility of a ‘Michelassi’ stricturoplasty. At laparotomy, 100 cm of diseased distal small bowel was identified, with multiple strictures and aneurysmal-type dilatations extending up to 10 cm from the ileocolic junction. The proximal 150 cm of small bowel was normal. Due to the length of diseased bowel, a Michelassi stricturoplasty was performed. The diseased bowel was divided into two 50 cm portions and the mesentery partially divided. Unsurprisingly, the mesentery was friable and suture ligation of vessels was required to achieve haemostasis. A longitudinal enterotomy was performed on the anti-mesenteric surface of the bowel and a side-to-side isoperistaltic anastomosis was performed using interrupted 3-0 PDS sutures to the inner and then the outer walls (Figs 1 and 2). This four hour stricturoplasty required a total of 139 needles. The patient was managed with complete gut rest with nasogastric decompression, parenteral nutrition and octreotide for the first week before introduction of fluids. His admission was complicated by central line sepsis on Day 8; however, he had no intra-abdominal problem. He was transferred to a rural hospital on Day 10 where he was managed for pulmonary embolus and discharged on Day 14 on rivaroxaban and weaning prednisone. He was subsequently commenced on infliximab and had no recurrence of obstructive symptoms at one year follow-up.
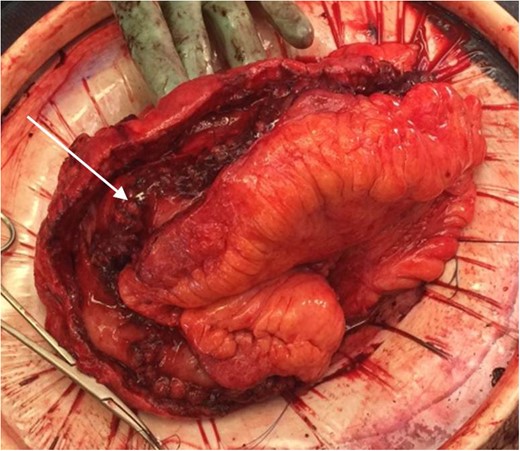
Completed posterior wall of the Michelassi stricturoplasty showing internal suture line (arrow).

Completed Michelassi stricturoplasty for the 100 cm of diseased bowel.
Case 2: A 23-year-old gentleman with a 7-year history of Crohn's disease and previous resection of 45 cm of jejunum presented with small bowel obstruction. Magnetic resonance enterography identified three fibrostenotic lesions, the largest of which was 10 cm long. The patient underwent laparoscopic adhesiolysis and mobilization of the small bowel, which was externalized through a small midline incision. Twelve small bowel strictures were identified using a Foley catheter passed through an enterotomy at an obvious stricture. A Heineke-Mikulicz stricturoplasty was performed at each point using interrupted 3-0 PDS sutures (Fig. 3). The patient had an uncomplicated postoperative recovery and was later commenced on adalimumab, with no further obstructive symptoms at one year follow-up.

DISCUSSION
The choice of stricturoplasty technique depends on stricture length. The Heineke-Mikulicz stricturoplasty is suitable for short strictures up to 10 cm and is used in over 80% of cases. It involves a single enterotomy with transverse closure [4, 6, 7]. For strictures 10–25 cm in length, the Finney stricturoplasty is appropriate. This involves folding the strictured segment into a U, creating a longitudinal enterotomy and anastomosing the adjacent bowel edges to form a blind pouch [4, 6, 7, 8]. For strictures >20 cm, entero-enterostomy such as the Michelassi stricturoplasty (described above) may be used. A variation of this technique is the Poggioli modification, where the diseased bowel is anastomosed to non-diseased bowel [9]. This is a faster anastomosis with reduced rates of early re-stenosis at the two ends of the stricturoplasty, however, it puts a strictures’ length of healthy bowel at risk [9].
Complications after stricturoplasty include sepsis (fistula, anastomotic leak or abscess) in 4% and stricture recurrence in 23% (3% at the stricturoplasty site and 20% at other sites) [4, 6]. Re-operation rates for recurrent strictures are comparable for both stricturoplasty and resection [4]. Carcinoma at the stricturoplasty site is a potential risk, however, overall incidence is low, with only two cases reported in a meta-analysis of 1112 patients [6].
The two cases described demonstrate that stricturoplasty is an effective bowel-sparing surgical option for stricturing Crohn's disease and can be safely performed in patients with widespread small bowel involvement. Stricturoplasty avoids the need for extensive bowel resection and the metabolic complications associated with short bowel syndrome.
CONFLICT OF INTEREST STATEMENT
None declared.



