-
PDF
- Split View
-
Views
-
Cite
Cite
Amal Ben Dahman, Philippe David, Nicolas Massager, Samuel Leistedt, Gwenolé Loas, A marsupialized retrovermian arachnoid cyst and psychotic symptoms, Journal of Surgical Case Reports, Volume 2017, Issue 8, August 2017, rjx162, https://doi.org/10.1093/jscr/rjx162
Close - Share Icon Share
Abstract
In this article, we report a male patient that developed psychotic symptoms after the excision of an arachnoid cyst from the posterior fossa detected by magnetic resonance and subsequent clinical improvement after anti-psychotic treatment.
INTRODUCTION
This case report shows the onset of psychotic symptoms according to DSM-IV after an arachnoid cyst surgery in the posterior fossa.
The patient is a 26-year-old man with higher education who consulted because of ongoing tinnitus. An early assessment revealed the presence of an arachnoid cyst at the posterior fossa level.
Conservative management was initially recommended but as the symptoms persisted, surgery was decided upon. The day after the surgery, the patient was presenting referential delusions, anxiety, incoherence of thought and speech. Therefore, he was administered anti-psychotics and after a few weeks he showed self-consciousness and all of the psychotic symptoms disappeared.
CASE REPORT
The patient is a 26-year-old man with higher education. He consulted because of ongoing tinnitus. An initial assessment using brain magnetic resonance imaging (MRI) revealed the presence of an arachnoid cyst at the posterior fossa level, located posterior to the cerebellum. It had a marked mass effect on the cerebellum and also extended bilaterally. Intracranial pressure was unaltered. The neurosurgical department recommended avoiding surgical intervention and suggested a follow-up of the cyst by MRI in 6 months’ time. However, as the symptoms persisted (ringing in the ears and some balance disorder when he turned his head when lying down), surgical excision of the cyst was scheduled. The patient was operated on by marsupialization for an arachnoid cyst in the posterior fossa.
The operation was carried out under general anesthesia. Two grams of Cefazolin were administered intraoperatively before craniotomy. After craniotomy, the dura was opened and a typical arachnoid cyst was discovered, with elevated internal pressure. The cyst was widely marsupialized, the dura was closed and the craniotomy was repaired. Then the patient was transferred to the post-recovery room and then directly to the Intensive Care ward for control. Post-surgical treatment consisted of Paracetamol 1 g four times a day and tramadol chlorhydrate 50 mg if deemed necessary for pain.
After the cyst was excised, the patient's bilateral tinnitus disappeared. However, he developed referential and bizarre delusions, anxiety, incoherence of thought and speech, delusional ideas, alteration of social behavior and mistrust. Nevertheless the patient had no negative thoughts, no cognitive impairment (the Mini-mental State Examination was normal: 28/30) and no aggressive behavior. He experienced no auditory or visual hallucinations.
The patient had no personal history of substance abuse. However, family medical history did include an older brother with schizophrenia. The day after the surgery, the patient ran away from the hospital's intensive care unit, he was caught though and hospitalized, against his will, in the Psychiatry Department.
He was prescribed risperidone 3 mg once daily in the evening with paroxetine 30 mg daily in the morning. Quetiapine fumarate 300 mg was given when the patient presented anxiety symptoms.
The post-surgical nuclear magnetic resonance showed the presence of extra-cranial fluid collection next to the craniotomy area, measuring 3 cm craniocaudal and 10 mm thick.
The pre- and post-surgical nuclear magnetic resonance results did not differ except for the track of marsupialization.
A few weeks later, the patient showed self-consciousness and could see the incoherence of his prior beliefs. Thus, he was discharged after 1 month of hospitalization.
DISCUSSION
Arachnoid cysts are congenital lesions of the arachnoid membrane that are expanded by the secretion of cerebrospinal fluid (CSF). They appear on both computed tomography (CT) and MRI as sharply marginated, homogeneous masses with a signal identical to CSF [1].
Radiological differentiation of arachnoid cysts from Dandy–Walker malformation is assessed by determining whether the cyst is an enlarged fourth ventricle (Dandy–Walker malformation), is in communication with the fourth ventricle (Dandy–Walker complex), or is isolated from the surrounding subarachnoid space (arachnoid cyst) [1].
In this case, the radiological presentation was in favor of the diagnosis of a retrovermian arachnoid cyst and not a mega-cisterna magna (Fig. 1). This was further confirmed by the peroperative discovery of a typical arachnoid cyst with an arachnoid membrane, which was widely opened during cyst marsupialization.
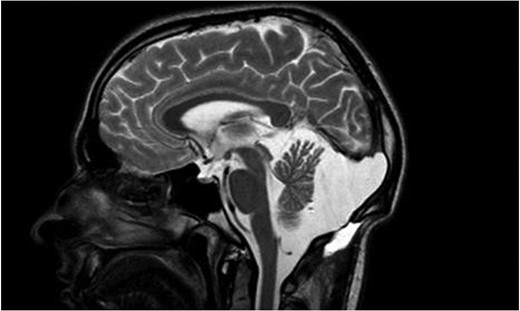
Sagittal T2 weighted image showing a marsupialized retrovermian arachnoid cyst.
There usually is an indication for surgery when there are symptoms of increased intracranial pressure, seizures, focal neurologic deficits or cognitive impairment. And thus, surgical options include craniotomy for partial or complete cystectomy [2].
In this patient's clinical picture, the psychotic symptoms appeared after the surgery despite a good recovery of neurologic symptoms and a reduction in mass effect on the cerebellum.
In this case, it could not have been a substance-induced psychotic disorder because there was no history of substance abuse or dependence and urine toxicology was negative.
The insidious onset of psychotic symptoms could have been due to the stress of the operation. It could not have been a brief psychotic disorder because, in that case, the duration is generally shorter, i.e. at least a day and no more than a month. Furthermore, a few months later, the patient stopped taking his anti-psychotic treatment and had a second psychotic episode with the same symptoms suggesting the onset of schizophrenia.
Thus, perhaps another mechanism had been at work in the onset of psychotic symptoms. For instance, anesthetic drugs (propofol and sufentanil) used during the operation could have precipitated symptoms in this young person with a familial predisposition. However, there are a number of reports on this and in one of these reports, the authors suggest that ketamine, propofol and fentanyl decrease the frequency of post-operative psychosis emergence. This was, however, not the case in our report [3].
The psychotic symptoms could have been due to cerebellar-lesion during the surgery as the lesions of the posterior lobe of the cerebellum result in cognitive symptoms, while the vermis has been shown to be implicated in patients with behavioral-affective disturbances [4].
In addition, posterior fossa syndrome is characterized by a range of linguistic, cognitive and behavioral-affective disturbances that may develop after etiologically different lesions of the cerebellum [5].
The authors postulate that even a less extensive cerebellar lesion, such as a ‘mega-cisterna magna’, can be associated with psychosis [6].
In conclusion, the limbic cerebellum corresponds with the posterior vermis; lesions lead to psychiatric disorders with alterations of social and emotional behavior [7].
CONFLICT OF INTEREST STATEMENT
None declared.



