-
PDF
- Split View
-
Views
-
Cite
Cite
Phong Jhiew Khoo, Stephen Jacob, An omental fibroma resembling a testicular tumour but presented as an irreducible inguinal hernia, Journal of Surgical Case Reports, Volume 2017, Issue 8, August 2017, rjx161, https://doi.org/10.1093/jscr/rjx161
Close - Share Icon Share
Abstract
We present a case of omental fibroma, which posed a surgical diagnostic dilemma. Primary tumours of the omentum are uncommon, and omental fibromas account for 2% of these. The rarity of omental fibroma and paucity of available information hamper an accurate diagnosis. In this particular case, the diagnostic process was misleading. The history was classical of an irreducible inguinal hernia, but the physical examination and imaging studies were suggestive of a testicular tumour. However, intraoperatively, an omental tumour and a normal testicle were found in the scrotum. Histopathological examination proved the tumour to be a fibroma. The presentation of an omental fibroma in an inguinal hernia sac had never been reported in literature. Due to the rarity of such cases, a thorough history, detailed examination, and objective investigation are the pillars to attain the correct diagnosis.
INTRODUCTION
Primary tumours of the omentum are uncommon, and omental fibromas account for 2% of these [1–5]. Pre-operatively, omental fibromas are seldom diagnosed correctly [2, 6]. The rarity of omental fibroma and the paucity of available information hamper making an accurate diagnosis [2, 4].
We recently came across a case that was misleading to our diagnostic process. The history was classical of an irreducible inguinal hernia but the physical examination and imaging studies were suggestive of a testicular tumour. However, intraoperatively, an omental tumour and a normal testicle were found in the scrotum. Histopathological examination proved the tumour to be a fibroma.
The presentation of an omental fibroma in an inguinal hernia sac had never been reported in literature. Due to the rarity of such cases, a thorough history, detailed examination and objective investigation are the pillars to attain the correct diagnosis.
CASE REPORT
We present the case of a 51-year-old gentleman with an omental fibroma. Initially, he sought medical attention at a primary healthcare centre for his chief complaint and was subsequently referred to our general surgical clinic for further consultation and management. He complained of right scrotal swelling occurring for the past 4 months, and the swelling was gradually increasing in size. He also described the swelling as reducible in the first month but subsequently irreducible. He did not experience any pain, denied any urinary tract symptoms, and claimed no alteration in bowel habits. No family history of malignancy was identified, and he denied experiencing any constitutional symptoms, such as weight loss, decreased appetite, fatigue or malaise.
Upon examination, we noted there was a huge right scrotal mass measuring roughly 10 cm × 7 cm × 7 cm. The mass was partially reducible, firm and hard in consistency and non-tender upon palpation. The normal right testicle was not appreciated. Examination of the external genital was normal.
We proceeded with an ultra-sonographic examination of the scrotum, which revealed a heterogeneous mass within the right scrotal sac measuring 7.0 cm × 6.2 cm. The normal right testicle was not seen (Fig. 1). The features were pointing towards a right testicular tumour. Thus, a computed tomographic (CT) scan was ordered, which revealed a right inguinal hernia containing greater omentum and a heterogeneous mass suggestive of a right testicular tumour as seen on the ultrasonography (Figs 2 and 3).
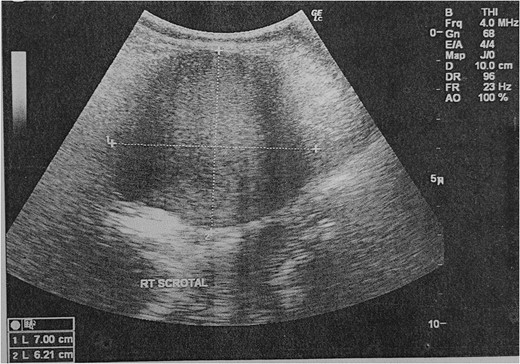
Ultrasonography of the scrotum showing a heterogeneous mass within the right scrotal sac.
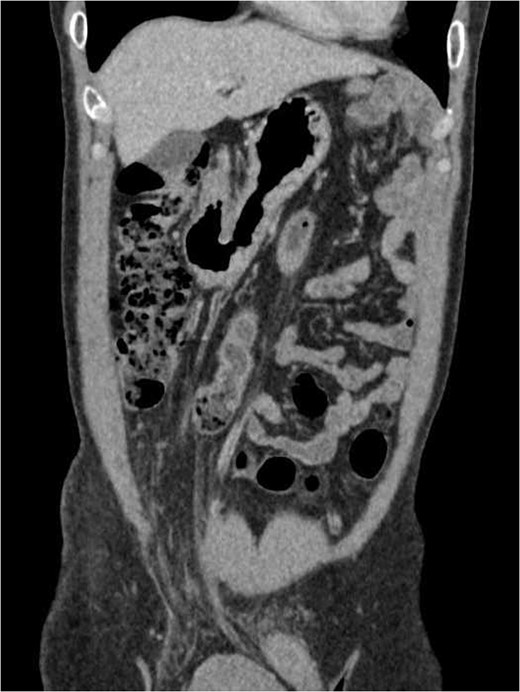
Coronal view of the thorax and abdomen CT scan showing a right inguinal hernia containing greater omentum.
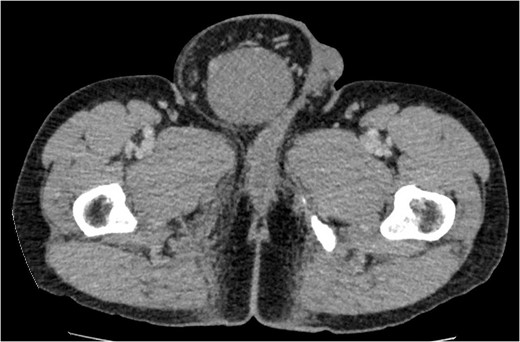
Cross-sectional view of the lower abdomen CT scan revealed a right inguinal hernia containing the greater omentum and a heterogeneous mass.
Tumour markers including alpha-fetoprotein (αFP), carcinoembryonic antigen (CEA) and beta human chorionic gonadotropin (βHCG) of the patient were within normal range. The nominal values are displayed in Table 1.
| Tumour markers . | Serum level . | Normal range . |
|---|---|---|
| Alpha-fetoprotein (αFP) | 3.15 IU/ml | 0.5–11.3 IU/ml |
| Carcinoembryonic antigen (CEA) | 2.24 ng/ml | 0.2–0.5 ng/ml |
| Beta human chorionic gonadotropin (βHCG) | <0.100 mIU/ml | 0.100–5.3 mIU/ml |
| Tumour markers . | Serum level . | Normal range . |
|---|---|---|
| Alpha-fetoprotein (αFP) | 3.15 IU/ml | 0.5–11.3 IU/ml |
| Carcinoembryonic antigen (CEA) | 2.24 ng/ml | 0.2–0.5 ng/ml |
| Beta human chorionic gonadotropin (βHCG) | <0.100 mIU/ml | 0.100–5.3 mIU/ml |
| Tumour markers . | Serum level . | Normal range . |
|---|---|---|
| Alpha-fetoprotein (αFP) | 3.15 IU/ml | 0.5–11.3 IU/ml |
| Carcinoembryonic antigen (CEA) | 2.24 ng/ml | 0.2–0.5 ng/ml |
| Beta human chorionic gonadotropin (βHCG) | <0.100 mIU/ml | 0.100–5.3 mIU/ml |
| Tumour markers . | Serum level . | Normal range . |
|---|---|---|
| Alpha-fetoprotein (αFP) | 3.15 IU/ml | 0.5–11.3 IU/ml |
| Carcinoembryonic antigen (CEA) | 2.24 ng/ml | 0.2–0.5 ng/ml |
| Beta human chorionic gonadotropin (βHCG) | <0.100 mIU/ml | 0.100–5.3 mIU/ml |
We consulted the urology team regarding this case. They reviewed the patient and concurred with our findings. Soon after, an elective right orchiectomy was planned for the patient. Intraoperatively, the right testicle was found to be normal in size and appearance, but there was a hernia sac containing omentum and a tumour with firm consistency (Fig. 4). The omental mass was removed, and the right inguinal hernia was repaired. Subsequent histopathological examination of the mass confirmed a benign omental fibroma.

Picture of the omental mass within the hernia sac (left), right testicle (middle) and left testicle in the scrotal sac.
The patient had an uneventful recovery. He remained well with no recurrence of the inguinal hernia.
DISCUSSION
Metastatic tumours of the omentum are more frequently seen compared to tumours originating from the omentum [1]. Even with widespread use of non-invasive imaging studies, incidental findings of such tumours remain relatively low [3, 4]. Only a handful of cases describing omental fibromas were reported, and all of those were discovered within the abdominal cavity [1, 2, 4, 5].
Essentially, fibromas are well-circumscribed tumours made up of dense collagen bundles with variable numbers of mature fibroblasts [2, 4, 5]. Fibromas are usually limited to their origin, despite the vast distribution of connective tissue throughout the human body [2, 4, 5]. They usually present as small, encapsulated, and firm tumours that are pearly grey on cross section [2, 4, 5]. Fibromas are composed of typical spindled fibroblasts that are closely packed with collagen [2, 5]. Histopathologically, our case shared similar features as described above.
Radiological or imaging studies, such as an ultrasonography, CT scan and MRI, can demonstrate proliferation of fibrous tissues and evaluate the relationship between the tumour and the surrounding structures [1, 4, 7]. Such investigations can provide meaningful input in making a diagnosis but are not sufficiently typical to be diagnostic [2, 4, 7]. Even with a pathognomonic radiological feature, such as multiple cystic areas and enhanced solid areas of a leiomyosarcoma, such investigations are not adequate in making a pre-operative diagnosis based solely on imaging studies [2, 4]. In our case, both the ultrasonography and CT scan were performed, which identified a heterogeneous mass in the right scrotal sac. The findings were not sufficient in making the diagnosis of omental fibroma. Besides that, the imaging studies also revealed a right inguinal hernia and were unable to appreciate a normal right testicle, which further swayed our diagnosis towards a right testicular tumour.
Currently, no studies have been carried out to assess the utility of fine-needle biopsy in the diagnosis of an omental tumour; thus, no objective data are available to support or deny the usage [1, 2, 4]. Ultimately, surgical resection not only provides the histopathological diagnosis but also serves as definitive management because fibromas rarely recur and never metastasize [2, 4]. As in this case, resection of the omental fibroma was performed, and the hernia defect was repaired.
The most common presentation of a testicular tumour is the gradual painless enlargement of the testicle [8]. Physical examinations of the patient raised clinical suspicion of a testicular tumour. The history was suggestive of an irreducible hernia, but it also can be perceived as a painless gradual growing mass in the scrotum. There was similar presentation reported by Gatt et al. [9] in a case report in which they described a 73-year-old gentleman who presented with a painless gradual enlargement of a right groin mass over a period of 6 months, and clinical examination demonstrated an enlarged right testicle with clinical suspicion of an irreducible hernia.
Ultimately, due to the rarity of such cases and variable presentations, a thorough history, detailed examination, and objective investigation are the pillars to attain the correct diagnosis of an omental fibroma.
CONFLICT OF INTEREST STATEMENT
None declared.



