-
PDF
- Split View
-
Views
-
Cite
Cite
Daichi Kitaguchi, Masanao Kurata, Osamu Shimomura, Tatsuya Oda, Nobuhiro Ohkohchi, Gallbladder bleeding associated with microscopic polyangiitis: a case report, Journal of Surgical Case Reports, Volume 2017, Issue 8, August 2017, rjx159, https://doi.org/10.1093/jscr/rjx159
Close - Share Icon Share
Abstract
A 71-year-old male who had a 6 years history of microscopic polyangiitis (MPA) was admitted to our hospital with a chief complaint of upper abdominal pain and nausea. Abdominal contrast-enhanced CT revealed extravasation of contrast medium in the gallbladder, and the patient was diagnosed with gallbladder bleeding. Although we started conservative treatment, anemia, hypotension and tachycardia had progressed gradually. Therefore, we performed emergent laparoscopic cholecystectomy on the following day. Intraoperative findings showed a remarkably distended gallbladder due to interior clots; however, the cholecystitis itself was not significant. Histopathological findings showed infiltrations of inflammatory cells around the blood vessels and vascular rupture. The postoperative course was uneventful. MPA is a type of ANCA-associated vasculitis. To the best of our knowledge, this is the first report of gallbladder bleeding associated with MPA. Spontaneous hemostasis cannot be expected, instead, surgical treatment must be performed promptly.
INTRODUCTION
Gallbladder bleeding is a rare condition that occurs in fewer than 1% of upper gastrointestinal bleeding cases. Although the major cause of gallbladder bleeding is hemorrhagic cholecystitis, the condition can also develop from vasculitis secondary to systemic collagen disease. Here, we report a case of gallbladder bleeding associated with microscopic polyangiitis (MPA).
CASE REPORT
A 71-year-old male was admitted to the internal medicine department of our hospital with a chief complaint of upper abdominal pain and nausea. He had been an outpatient of the rheumatology department since he was diagnosed with MPA through a lung biopsy 6 years ago. Hematological findings showed elevation of hepatobiliary enzyme. The patient was diagnosed with passage of a common bile duct stone because the symptoms disappeared spontaneously. On hospital Day 6, he was introduced to the surgical department because his upper abdominal pain had relapsed.
The patient’s vital signs were normal, with no fever, and the pain was diffuse, with no tenderness. Hematological findings showed mild inflammation (WBC 10 700/μl, CRP 1.07 mg/dl) and elevation of hepatobiliary enzyme (AST 69 U/l, ALT 370 U/l, LDH 228 U/l, ALP 982 U/l, γ-GTP 518 U/l), but no jaundice was observed (T-Bil 0.9 mg/dl). Abdominal ultrasonography revealed gallbladder distention, but no gallstones, fluid surrounding the gallbladder, gallbladder wall thickening or sonographic Murphy’s sign were observed. Abdominal contrast-enhanced CT revealed extravasation of contrast medium in the gallbladder, and the patient was diagnosed with gallbladder bleeding (Fig. 1).

Abdominal contrast-enhanced CT. Abdominal contrast-enhanced CT revealed extravasation of contrast medium in the gallbladder.
We expected spontaneous hemostasis and started conservative treatment because the vital signs were stable and cholecystitis was not found. However, anemia, hypotension and tachycardia had progressed gradually, and active gallbladder bleeding appeared to be sustained. Accordingly, we performed emergent laparoscopic cholecystectomy on the following day.
Intraoperative findings showed a remarkably distended gallbladder due to interior clots; however, the cholecystitis itself was not significant. Few adhesions occurred around the gallbladder, and the wall of the gallbladder was edematous. The gallbladder was easily dissected from the liver bed because the subserosal layer of the gallbladder wall could be readily divided into inner and outer layers. The surgery time was 128 min, and the intraoperative blood loss was 180 ml (including the clots).
Histopathological findings showed necrosis and bleeding of the gallbladder wall in places. At the area of the gallbladder with bleeding, infiltrations of inflammatory cells around the blood vessels and vascular rupture was seen in the muscularis propria (Fig. 2a and b). However, little inflammatory cell infiltration was observed in the areas of the gallbladder without bleeding (Fig. 2c).
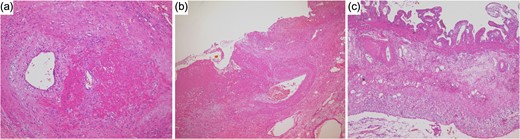
Histopathological findings. (a) At the area of the gallbladder with bleeding, infiltrations of inflammatory cells around the blood vessels was seen in the muscularis propria. (b) Vascular rupture was seen in the muscularis propria. (c) Little inflammatory cell infiltration was observed in the areas of the gallbladder without bleeding.
The postoperative course was uneventful, with no major complications. The patient was transferred to internal medicine for treatment of MPA on postoperative Day 2.
DISCUSSION
Gallbladder bleeding is a rare condition that occurs in fewer than 1% of upper gastrointestinal bleeding cases. The first case of gallbladder bleeding was reported by Sandblom [1]. Although the causes of gallbladder bleeding are diverse, the major cause besides iatrogenesis, trauma and bleeding from tumors is hemorrhagic cholecystitis [2].
The main pathogenetic mechanism of hemorrhagic cholecystitis begins with the development of acute gallbladder inflammation. Necrotizing infection of the mucosa and erosion formation is induced due to the progression of inflammation, and blood vessels in the gallbladder wall are injured. The diagnosis and treatment policy in these cases are easily decided because the clinical findings are not significantly different from those of typical cholecystitis.
The other pathogenetic mechanism of hemorrhagic cholecystitis occurs due to gallbladder bleeding. Clots obstruct the cystic duct or increase the internal pressure of the gallbladder, the gallbladder wall experiences ischemic change, and secondary cholecystitis develops. In these cases, as in our case, it is difficult to decide the diagnosis and treatment policy because the clinical findings differ from those of typical cholecystitis at the early stage.
MPA is a type of ANCA-associated vasculitis (AAV). Pathologically, the condition is defined as necrotizing small-vessel vasculitis without granuloma, and no deposition of immune complexes occurs on the blood vessel walls. Although the etiology is unknown, an autoimmune disorder is thought to involved because myeloperoxidase antineutrophil cytoplasmic antibody (MPO-ANCA) is detected at a high rate. [3, 4].
Although digestive organ disorders secondary to MPA are relatively common, vasculitis of the gallbladder secondary to MPA is extremely rare [5]. Only seven previous reports of this condition have been reported [5–8], and our case is the first report of gallbladder bleeding secondary to MPA.
Spahn et al. [9] reported a case of hemobilia associated with MPA similar to our case. In their case, a pseudoaneurysm was formed secondary to MPA at the branch of the right hepatic artery, and this pseudoaneurysm perforated the intrahepatic bile duct. Therefore, the cause of hemobilia associated with MPA included both gallbladder bleeding and an arteliobilliary fistula. Incidentally, transarterial embolization was performed to obtain hemostasis. In our case, abdominal contrast-enhanced CT revealed extravasation of contrast medium in the gallbladder, making diagnosis simple. It is important to confirm a bleeding point, make a diagnosis, and decide a treatment policy by combining multiple methods of examination in cases of hemobilia associated with systemic vasculitis.
Koizumi et al. reported a case of gallbladder bleeding associated with eosinophilic granulomatosis with polyangiitis, which is the other type of AAV [10]. Interestingly, the clinical course and pathological findings of their case and our case have many points in common. In both cases, although conservative treatment was initially started because the vital signs were stable and the clinical findings differed from those of typical acute cholecystitis, an emergent operation was performed on the following day due to the progression of anemia. Furthermore, in both sets of pathological findings, although the blood vessels were injured, inflammatory changes in mucosa were unremarkable.
For cases in which the hemorrhagic legion is localized in the gallbladder, hemostasis can be obtained spontaneously by conservative treatment, and elective surgery for gallbladder bleeding is allowable [10]. However, spontaneous hemostasis is difficult to obtain in cases of gallbladder bleeding secondary to AAV. Therefore, surgical treatment must be performed promptly for gallbladder bleeding associated with AAV.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- anemia
- cholecystitis
- tachycardia
- inflammatory cells
- hypotension
- abdominal pain
- contrast media
- hemorrhage
- hemostatic function
- extravasation of diagnostic and therapeutic materials
- intraoperative care
- nausea
- rupture
- surgical procedures, operative
- abdomen
- gallbladder
- hemostasis procedures
- laparoscopic cholecystectomy
- microscopic polyarteritis nodosa
- anca-associated vasculitis
- conservative treatment
- chief complaint



