-
PDF
- Split View
-
Views
-
Cite
Cite
Yuko Miyazaki, Kenji Fukuda, Kazutoshi Fujita, Soh Nishimoto, Tomonori Terada, Ryu Wada, Yohei Sotsuka, Kenichiro Kawai, Masao Kakibuchi, Free flap transfer reconstruction in managing tongue carcinoma during pregnancy, Journal of Surgical Case Reports, Volume 2017, Issue 8, August 2017, rjx164, https://doi.org/10.1093/jscr/rjx164
Close - Share Icon Share
Abstract
Malignant oral cancers do not commonly occur in pregnant women. But when they do, the presence of a foetus and maternal physiological changes complicate and limit the treatment options. Risk benefit assessment and balancing of them are always important. A 33-year-old woman, who was 25 weeks pregnant, presented with a squamous cell carcinoma on her tongue. She was clinically staged II (T2, N0 and M0). Discussions between the patient, surgical teams and obstetricians agreed to continue her pregnancy while managing the tumour. Hemi-glossectomy and ipsilateral neck dissection was performed. Free antero-lateral thigh flap was transferred to reconstruct the tongue defect, successfully. The patient gave birth to a healthy baby afterward. She is tumour free for 6 years. Free flap reconstruction can be an option, even if the patient is pregnant.
INTRODUCTION
In managing tongue carcinoma, radical resection of the tumour and immediate reconstruction, if needed, can be called the first choice. Malignant oral cancers do not commonly occur in pregnant patients. But when they do, they are difficult to manage. The presence of a foetus complicates and limits the treatment options. In many cases, pregnant patients unwillingly elect to terminate their pregnancy, being addressed for the control of the malignant tumour. Here, we report our successful experience in managing pregnant woman with tongue cancer, by radical resection and free flap reconstruction.
CASE REPORT
A 33-year-old woman with a squamous cell carcinoma of the right lateral border of the tongue, who was 25 weeks pregnant (gravida 5 para 4). The lesion measured 23 × 8 mm2 (Fig. 1). Infiltration into tongue muscle was observed in MRI image (Fig. 2). The patient was staged as T2, N0 and M0. Discussion between surgical teams and obstetricians were held and agreed to continue her pregnancy while managing the tumour. Complete resection of the tumour was affirmed to be essential in controlling the cancer.

A 33-year-old pregnant woman presented with a carcinoma on her tongue. White arrow indicates the tumour.
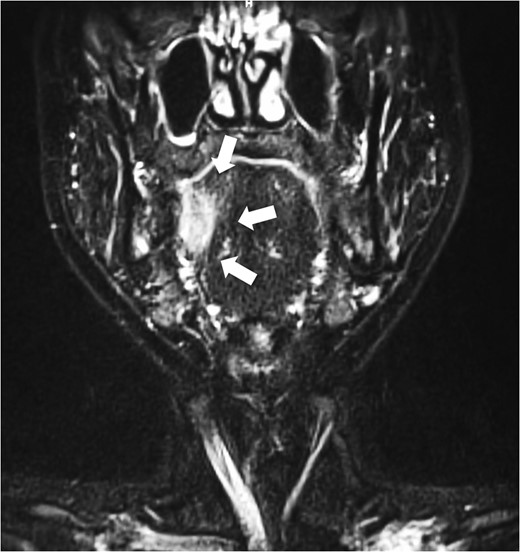
Pre-operative coronal MRI. Invasion into tongue muscle was observed. White arrow indicates the tumour.
The surgical treatment for this patient involved tracheostomy, hemi-glossectomy and right-sided selective neck dissection when the patient was in her 28th week of pregnancy. Throughout the surgery, the patient was given a continuous intravenous infusion of ritodrine hydrochloride (100 mg in 500 ml) in order to provide tocolysis and prevent premature labour. A tracheotomy was preformed and the patient underwent a modified rapid sequence induction using fentanyl, thiopentone and rocuronium bromide. Anaesthesia was maintained with sevoflurane. A continuous fentanyl infusion provided analgesia and paralysis was maintained with boluses of atracurium besylate. Obstetricians were standing by for unexpected delivery. A cardiotocograph was used to monitor the foetus. The tissue defect was reconstructed with an antero-lateral thigh flap (Figs 3–5). The descending branch of lateral circumflex femoral artery was anastomosed to her right facial artery. One comitant vein was anastomosed to her external jugular vein in end-to-end fashion with a 2.5 mm microvascular anastomotic device. The other comitant vein was anastomosed in the same way to a branch of internal jugular vein with a 2.0 mm coupler. Heparin-saline solution (5000 units in 100 ml) was used to irrigate the anastomotic sites. Systemic heparin administration was not done during the operation. Lidocaine (2%) was used as vasodilator. Prostaglandin E1 was not administered. The operation took 7 h and 40 min. Blood loss was estimated to be 340 ml and no blood transfusion was required. Throughout the operation, no remarkable incidents were noted on the electronic foetal monitoring.
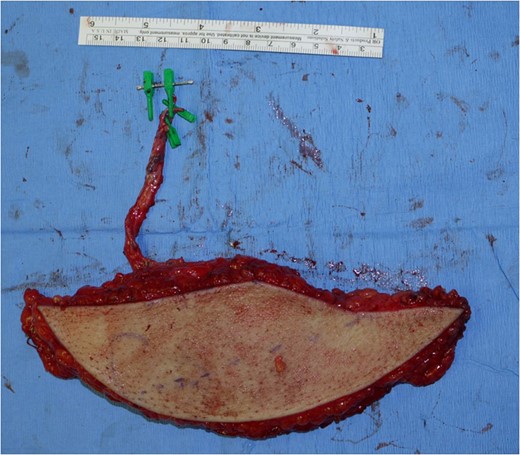
A free antero-lateral thigh flap was harvested from her right thigh.
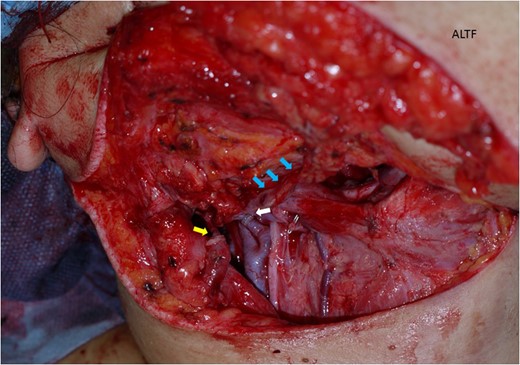
The antero-lateral thigh flap (ALTF) was transferred to her neck area. The descending branch of lateral circumflex femoral artery (blue arrows indicating) was anastomosed her right facial artery. A comitant vein was anastomosed to her external jugular vein in end-to-end fashion with a 2.5 mm microvascular anastomotic device (yellow arrow). The other comitant vein was anastomosed in the same way to a branch of internal jugular vein (white arrow).
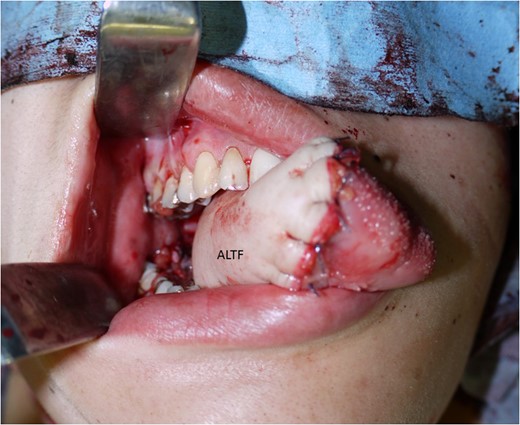
The antero-lateral thigh flap (ALTF) was pulled through, trimmed and sutured to fill the tongue defect.
Soon after the operation, uterine contractions and shortening of the cervix were noted. Tocolysis was successfully obtained with ritodrine. Post-operative prophylactic low molecular weight heparin was used to prevent thrombosis. For analgesia, continuous administration of fentanyl was done for 2 days, and 200 mg acetaminophen suppository was given after that. D-dimer test rose up to 12.6 μg/ml (normal level: below 0.4 μg/ml), and anti-thrombin 3 decreased to 74% (normal level: 80–120%) on the first post-operative day as extremal value. Symptomatically, no sign for thrombosis was observed. The transferred flap totally survived. Pathologically, surgical margin was negative and no metastasis was seen in lymph nodes. The patient was released from the hospital when she was in her 31st week of pregnancy.
Three months after the surgery (38 weeks and 6 days of gestation), the patient naturally delivered a healthy baby (birth weight was 2786 g). Post-operative chemotherapy and irradiation were not done. The patient is in good health without any sign of recurrence and metastasis of the tumour for 6 years. She has no disturbance in mastication and swallowing nowadays. She can speak normally without difficulty (Figs 6 and 7).
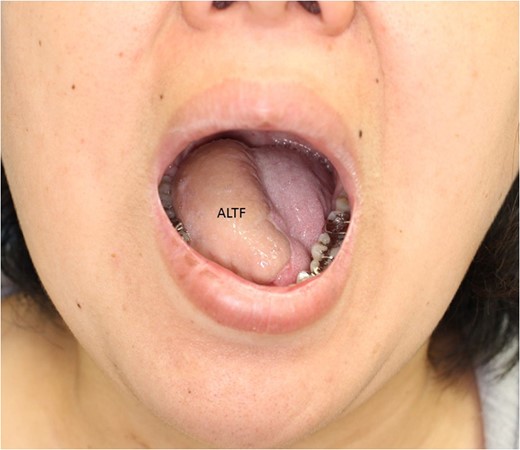

Two years after the operation, sticking out her tongue. She faces no difficulty in speaking, mastication and swallowing.
DISCUSSION
Approximately 1 per 1000 pregnant women will develop cancer [1]. Though, tongue cancer in this category is relatively rare. According to Murphy et al. [2], at the point of 2016, 33 cases of squamous cell carcinoma of the tongue during pregnancy has been reported in English literatures. Although, from the fact that there was only one case in the series reportedly chose termination of pregnancy, they mentioned that publication bias must be considered. If the gestation period is 34 weeks or further, cancer control may be begun after delivery.
Pregnancy triggers various physiologic changes that may impede surgery. During pregnancy, inflammatory immune response that might reject foetus is reduced. Concentrations of several hormones change, that alter cell-mediated and humoral immune response [3]. Although it is known that pregnant women respond differently to the presence of microorganisms or its products and the immune system is uniquely modulated, pregnancy should not imply more susceptibility to infection diseases [4].
Pregnancy is a state of hypercoagulation, that may reduce risk of haemorrhage during delivery and post-partum. Pulmonary thromboembolism is one of the main causes of maternal death [5]. Deep vein thrombosis rate is very high in pregnant women [6]. Hypercoagulative state is not a preferable condition for a free flap transfer. The risk of anastomotic thrombosis is heightened [7]. Microvascular anastomotic devices were used to anastomose veins, which is our routine procedure. With the device, it is not difficult to anastomose veins with mismatching diameter [8]. The polyethylene coupling rings will keep the anastomosed site open from outside of the vessels, that is another advantage of using them [8]. Systemic prostaglandin E1 administration was avoided, that may have adverse effect on the uterus. In fact, we have not been using prostaglandin E1 for routine free flap reconstructions, based on the lack of evidence for the efficacy [9]. Heparin was not administered before and during the operation, but was used post-operatively. Fortunately, we did not experience thrombosis, although lab data showed transient D-dimer rise and anti-thrombin 3 dip.
The patient, with T2, N0 and M0 (stage 2) disease, was a candidate for primary or post-operative radiotherapy. There are some radiotherapy reports for pregnant women with tongue cancer [2, 10]. Discussion with the patient concluded to avoid radiotherapy. She was not able to let go the fear for teratogenesis and further impacts on the foetus.
Treatment options in managing malignancy is varied not only by stage or gestation period but also by the patients and their families including social environment. There do exist many risks. Multidisciplinary approach with good communication is essential in making complex decisions. Free flap reconstruction does not have to be omitted from the optional procedures, merely because the patient is pregnant.
CONFLICT OF INTEREST STATEMNT
None declared.



