-
PDF
- Split View
-
Views
-
Cite
Cite
Basim Al Khafaji, Muhammad Umar Younis, Laparoscopic splenic cyst fenestration—a viable spleen preserving option, Journal of Surgical Case Reports, Volume 2017, Issue 8, August 2017, rjx154, https://doi.org/10.1093/jscr/rjx154
Close - Share Icon Share
Abstract
Cystic lesions of the spleen are a rare encounter in surgical practice and are broadly split into two categories: true and false, depending upon the presence of a defined epithelial lining. True cysts can further be broken down into parasitic and non-parasitic origins while false or pseudocysts tend to develop commonly after a traumatic event. We present here a 23-year-old female who came to the clinic with symptoms of abdominal fullness, early satiety and left flank pain which was diagnosed as a large splenic cyst after radiology confirmation. The patient was prepared and underwent laparoscopic splenic cyst fenestration successfully without any complications. Laparoscopic fenestration for benign uncomplicated splenic cysts is a viable alternative to splenectomy with low rates of recurrence and less patient morbidity along with the advantage of preservation of splenic function.
INTRODUCTION
True, non-parasitic cysts are usually congenital in origin with presentation in the younger age group and are commonly observed in the upper pole of the spleen [1, 2]. Even though the presentation of these cysts is quite rare, the frequency with which they are being diagnosed as incidental findings is increasing due to the fact that abdominal imaging techniques are improving and becoming more commonplace [3].
CASE REPORT
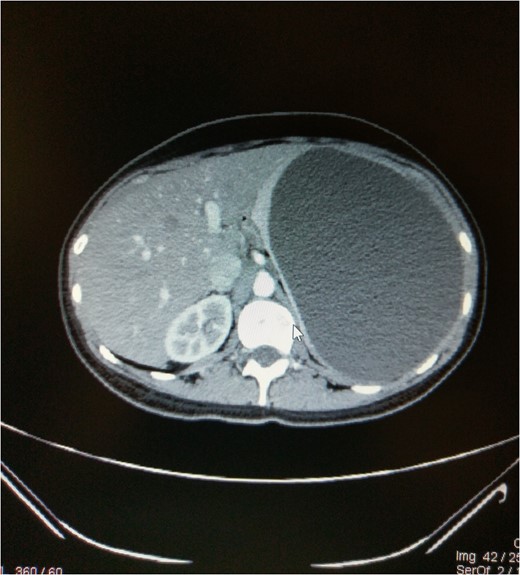
A 23-year-old female presented to the outpatient clinic of our hospital with complaints of abdominal fullness, early satiety, intermittent left upper quadrant abdominal pain and left flank pain for the last 3 months. No significant family history or history of trauma was described. Examination of the abdomen showed a non-tender enlarged mass in the left hypochondrium spanning upto the right iliac fossa. The report indicated a large space occupying lesion in the left upper quadrant of abdomen with probable origin being the spleen. A CT scan of abdomen and pelvis with IV contrast was advised for further evaluation which confirmed a 16.7 × 14.2 × 12.4 cm3 large splenic cyst on the upper outer pole with no intrinsic enhancement or internal septa, having a mass effect on the left kidney pushing it downwards and rotating it while putting a stretch on the left renal vessels (Figs 1 and 2). There was also a mass effect on the body and fundus of the stomach which explains the fullness and satiety by the patient. Serologic testing for Echinococcus was also performed and found to be negative.
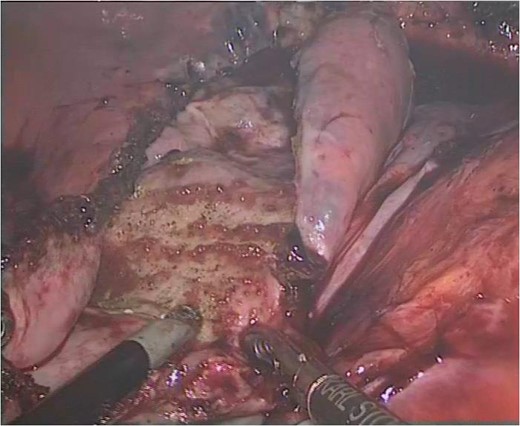
A decision to preserve as much of spleen as possible was undertaken and the patient was prepared for laparoscopic fenestration of the cyst. Preoperative vaccination against encapsulated microorganisms was carried out 2 weeks prior to surgery, in case an intraoperative situation prompted to go ahead with total splenectomy. The patient was placed in an improvised position being tilted 45° to the right lateral side with a sandbag under lumbar region to allow for placement of the first trocar avoiding the spleen. Veress needle CO2 insufflation was carried out to achieve a pneumoperitoneum at 14 mmHg via an incision in the left flank at the lateral border of rectus in the midclavicular line at the level of the umbilicus with an appropriate distance from the palpable edge of the spleen. Entry was gained into the abdominal cavity using 10 mm Visiport through the same incision and then three more working ports were inserted under direct vision: a 5 mm in the left anterior axillary line at the level of umbilicus, a 10 mm in the midline and a 10 mm in the left midaxillary line at appropriate triangulation distances of one another. An enlarged splenic cyst was seen with adhesions with the anterior abdominal wall. Dissection was initiated using the Harmonic Scalpel and the phrenicocolic, lienorenal and phrenicosplenic ligaments were divided to gain access to the cyst and allow mobilization. Once mobilized, aspiration was carried which allowed over 2 L of serous fluid to be withdrawn and aiding in further dissection with ease (Fig. 3). The cyst wall was then excised off the splenic parenchyma and the inner epithelial lining was cauterized using monopolar diathermy (Fig. 4). The excised cyst wall was removed using an endobag and specimen sent for histopathology. Irrigation and suction was further carried out before placing a 16 Fr penrose drain and omentum was packed in the splenic bed to prevent recurrence. The drain was removed after 48 h and patient was comfortably discharged on her second postoperative day. Pathology results were consistent with benign splenic epithelial cyst and the cystic fluid showed no evidence of malignant cells. The patient remains in good health and symptom free. A follow-up ultrasound done 3 months after surgery showed no evidence of cyst recurrence.
DISCUSSION
The infrequent appearance of non-parasitic splenic cysts in the field of surgery has precluded emergence of any standard management strategy for it. The previous accepted standard of care was splenectomy, but the likelihood of developing overwhelming postsplenectomy infection and fatal sepsis, has pushed surgeons to adapt to various techniques to preserve as much viable splenic tissue as possible [4].
The clinical presentation of these cysts is non-specific in uncomplicated cases. Cysts growing to larger sizes can present with a palpable mass in the left upper quadrant of the abdomen with vague sensation of fullness and pain attributed to the distension of its capsule [1, 5]. Other symptoms that may progressively appear are those that present as a result of pressure on the neighboring organs and may include distension, early satiety, vomiting, flatulence, persistent cough due to irritation of the diaphragm, pleuritic pain and renal symptoms due to compression of the left kidney [5, 6]. Complications like hemorrhage, infection and rupture causing peritonitis are possible but are fortunately rare [7].
Although ultrasonography may be able to distinguish between cystic and solid components, the mainstay of radiological diagnosis in such cases is CT scan which not only provides information concerning cyst morphology, location with respect to splenic hilum, cystic fluid composition, it also allows differentiation between parasitic and non-parasitic origins [3, 8]. Traditionally, the treatment strategies for splenic cyst have been either partial or total splenectomy. With the advent of laparoscopy, many surgeons have successfully attempted with quite success a minimally invasive approach to preserve splenic tissue. Watchful waiting with serial ultrasound surveillance is advocated for asymptomatic cysts <5 cm [9]. Other conservative options including percutaneous aspiration with or without injection of a sclerosing agent in the cavity have been tried but fell in disfavor because of high rates of recurrence [1].
Optimum spleen preserving modes of treatment include partial splenectomy, marsupialization, cystectomy, decapsulation and deroofing or fenestration [1, 10, 11]. Studies have led credence to the fenestration procedure showing acceptable rates of recurrence with the laparoscopic approach if as much as possible cyst wall is aptly excised so as to prevent reclosure of cyst [9, 12–14]. However, this type of management can be carried out only if the cyst is observed to be superficial and located at the poles. If the patient presents with a cyst located near the hilum or is intrasplenic, or if multiple cysts are present, a more assertive strategy should be undertaken in the form of total splenectomy [15]. The advantages of carrying out a laparoscopic modus operandi are evident as seen in other laparoscopic procedures namely shorter hospital stay, less pain, quicker recovery, cosmesis and enhanced patient satisfaction.


CONCLUSION
Laparoscopic fenestration for benign uncomplicated splenic cysts, where possible, is a viable alternative to splenectomy with low rates of recurrence and less patient morbidity and advantage of preservation of splenic function. It has been shown to be an effective treatment strategy with the benefits that come with minimally invasive approach.
SUPPLEMENTARY MATERIAL
Supplementary material is available at the Journal of Surgical Case Reports online.
CONFLICT OF INTEREST STATEMENT
None declared.



