-
PDF
- Split View
-
Views
-
Cite
Cite
Salil Umranikar, Sarvpreet Ubee, Graham Williams, Aggressive angiomyxoma of the perineum: a rare presentation in a male with 4 years follow up, Journal of Surgical Case Reports, Volume 2017, Issue 8, August 2017, rjx086, https://doi.org/10.1093/jscr/rjx086
Close - Share Icon Share
Abstract
Angiomyxoma are rare myxoid cells tumours that occur predominantly in women in the fourth decade. They are classified as the less aggressive superficial and the deeper aggressive variety commonly called aggressive angimyxomas. We report a rare perineal aggressive angiomyxoma in a 79-year-old male presenting with a painless perineo-scrotal mass. Radiological investigations confirmed a lobulated well-defined mass separate from the testicles and histology following wide local excision confirmed aggressive angiomyxoma. He remains recurrence free at 4 years of surveillance which is the among longest reported follow-up for perineal angiomyxoma.
INTRODUCTION
Angiomyxomas are soft tissue tumours that are exceedingly rare with about 150 cases being described in the literature. They are classified as, superficial and deep, with the latter characterized by aggressive local growth and a propensity to recur. Predominantly occurring in women, the vast majority of tumours occur within the vicinity of the lower pelvis commonly perineum, vulva, vagina or inguinal regions [1]. This case report details the rare presentation of a male presenting with an aggressive angiomyxoma of the perineum with a 4-year recurrence free follow-up, which to the best of our knowledge is the longest duration of follow up so far.
CASE REPORT
A 79-year-old male presented with a painless scrotal mass which he had noticed 10 days prior to presentation and denied any significant increase in size over this duration. He denied any urinary tract symptoms, haematuria, weight loss, night sweats or anorexia.
Examination revealed a non-tender 8 cm midline scrotal mass extending into the perineum with a smooth surface and a rubbery consistency. Both testis were normal on examination and distinctly separate from the mass. Rectal examination revealed a benign prostate with no other masses. There was no palpable inguinal lymphadenopathy.
An initial ultrasound confirmed a well-defined heterogenous encapsulated solid mass with internal vascularity. An abdominopelvic MRI revealed a 5.4 cm × 7.2 cm × 15.7 cm solid-cystic well-defined lobulated mass within the perineum separate from the testicles, adjacent to the penis and extending to the right ischial fossa and the obturator internus muscle (Fig. 1). Anteriorly the mass displaced the penile urethra and bulb and the anal sphincters without direct involvement (Fig. 2). There was no locoregional or para-aortic lymphadenopathy.
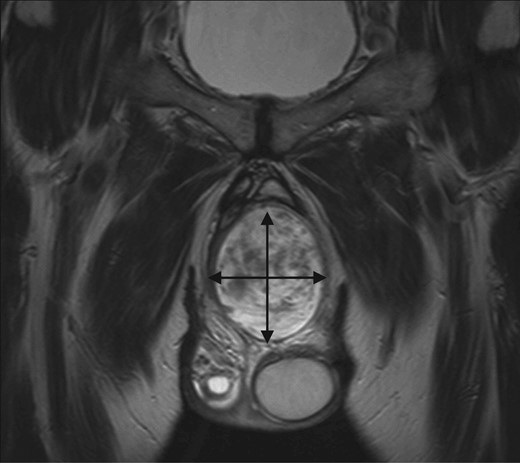
MRI abdomen and pelvis T2 weighted sequence coronal view demonstrating well-defined heterogeneous mass within the perineum.
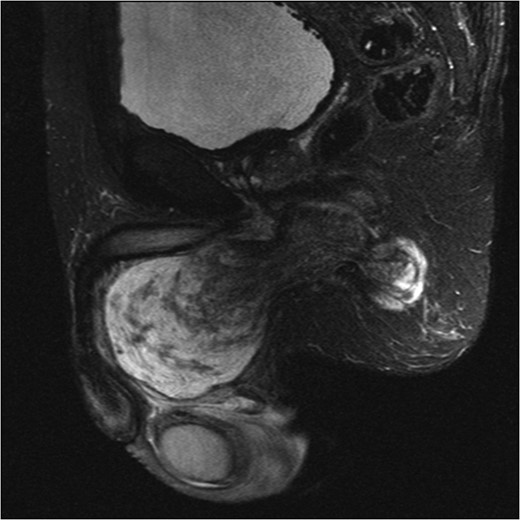
MRI abdomen and pelvis T2 weighted sequence sagittal view showing a predominantly cystic mass with scattered solid components within perineum.
Following multidisciplinary review, a wide local excision was performed. Intra-operatively, a large encapsulated tumour was found beneath the fascia extending to the base of the penis anteriorly along the urethra superiorly and toward the anus posteriorly. Histology revealed an aggressive angiomyxoma. At 4 years of regular surveillance, there has been no clinical or radiological signs of recurrence.
DISCUSSION
Aggressive angiomyxomas are rare tumours of myxoid/ mesenchymal cells that although benign, exhibit some ability to invade local surrounding tissue such as muscle and adipose tissue. They also display a tendency to recur necessitating prolonged surveillance.
Angiomyxomas tend to present as asymptomatic slow growing masses with a preponderance in women in fourth decade with M:F ratio of 6:1 [1]. Typically occurring within the pelvic and perineal tissues in both sexes, they have rarely been reported within the upper abdomen and in transplant kidneys as well [2].
Most cases usually present as an asymptomatic mass often being mis-diagnosed initially as other pathological swellings such as lipoma or cysts. The palpable and visible extent is often only the ‘tip of the iceberg’ and can extend considerably into deeper tissues, a fact best appreciated with imaging. Not uncommonly, pressure symptoms, pain, urinary obstructive symptoms, dyspareunia or bowel symptoms may predominate. Diagnosis is usually made following excision, although imaging characteristics have now been defined [3].
Radiological imaging is critical in assessing extent and surgical approach and in surveillance for recurrence. Ultrasonography usually demonstrates a cystic or hypoechoic lesion [3]. CT findings are non-specific but tumours exhibit attenuation values less than muscle and may demonstrate cystic components [2]. MR imaging is currently the mainstay with lesions usually hypointense on T1 weighted, hyperintense on T2 weighted and a characteristic ‘whorled’ appearance post Gadolinium contrast [3].
Macroscopically, tumours are typically fleshy, poorly encapsulated with adherence to surrounding tissues and often display areas of haemorrhage, necrosis and fibrosis [4].
Microscopically, cells with a spindled or stellate morphology appear within a matrix of wavy collagen. Cellularity is generally sparse and infiltration into fat, muscle and nerves may be seen [4]. The hallmark of aggressive angiomyxoma is vessels of varying calibre haphazardly scattered throughout the parenchyma. Mitotic figures are scarce [4]. Immunohistochemically, there are no specific markers, however, most aggressive angiomyxomas stain positive for desmin, smooth muscle actin, muscle-specific actin, vimentin and characteristically for oestrogen and progesterone receptors suggesting a hormonally driven basis for these tumours. Some tumours are positive for CD34, whereas S100 is invariably negative.
Genetically, translocations within the High Mobility Group A (HMGA2) have been frequently observed and may have a role in the future as a discriminatory marker [2].
Surgical excision is the mainstay for histological diagnosis and treatment with wide local excision being preferred where feasible. Larger more extensive tumours risk more extirpative surgery with accompanying significant morbidity. The risk of positive margins and recurrence is still undefined but a review of 111 cases showed no statistically significant difference in recurrence rates [5].
Chemotherapy and radiotherapy have at present an undefined and limited role while hormonal therapy may have an increasing primary or adjuvant role in hormonally responsive tumours.
In conclusion, aggressive angiomyxomas are rare and rarer still in males. Management includes wide local excision. Prognosis is generally good although recurrence rates vary between 25 and 50% with the majority recurring within 5 years. At the longest reported follow-up of 4 years for perineal angiomyxoma, in our patient no clinical or radiological recurrence has been noted.
CONFLICT OF INTEREST STATEMENT
None of the contributing authors have any conflict of interest, including specific financial interests or relationships and affiliations relevant to the subject matter or materials discussed in the article.



