-
PDF
- Split View
-
Views
-
Cite
Cite
Yohei Kawatani, Hirotsugu Kurobe, Yoshitsugu Nakamura, Yuji Suda, Takaki Hori, Aortic rupture due to radiation injury successfully treated with thoracic endovascular aortic repair, Journal of Surgical Case Reports, Volume 2017, Issue 5, May 2017, rjx092, https://doi.org/10.1093/jscr/rjx092
Close - Share Icon Share
ABSTRACT
Thoracic endovascular aortic repair (TEVAR) has been reported to be an effective treatment option for aortic emergencies. However, there are few reports about TEVAR for aortic rupture due to radiation injury. A 54-year-old man presented with haemoptysis. He had a history of lung cancer, which had been treated with chemotherapy and radiation therapy (72 Gy/16 times) 3 years previously, and the cancer lesion did not progress. On chest radiography, pneumonia was suspected in the radiated lesion. However, after admission, he presented with back pain, progressive anaemia and hypotension. Enhanced computed tomography revealed extravasation of contrast medium in the distal aortic arch. He was diagnosed with aortic rupture due to radiation injury. TEVAR was performed. He was extubated one day after the operation, and the haemoptysis disappeared. He was discharged from the hospital without any complications. He is well 1 year after the surgery, without aortic disease progression or lung cancer recurrence.
BACKGROUND
Rupture of the aorta after radiation exposure is a relatively rare but life-threatening complication of radiation therapy. The complication was reported as early as 1962 by Marcias-Rojas and Castro [1]. The treatment of aortic rapture involves surgery for repairing the damaged vessel. Currently, thoracic endovascular therapy is the standard option for aortic diseases and has been reported to be useful in acute aortic conditions, including aortic aneurysm rupture [2]. Here, we report a case in which we performed thoracic endovascular aortic repair (TEVAR) for aortic rupture due to radiation injury.
CASE PRESENTATION
A 54-year-old man presented to a rural hospital with a compliant of haemoptysis. On examination, his vital signs were normal.
He had a history of lung cancer, with invasion to the mediastinum and left subclavian artery. The cancer had been treated with chemotherapy and radiation therapy (72 Gy/16 times) 3 years prior to the presentation, without progression after the treatment. Additionally, tumour markers became negative after completion of the treatment and there was no aortic aneurysm.
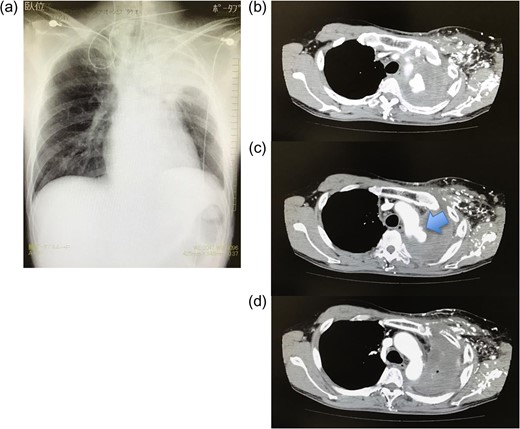
(a) Chest radiography on admission. Consolidation is observed in the left upper lobe. (b–d) Enhanced computed tomography after admission. Extravasation of contrast medium is observed in the distal aortic arch. The entry point is identified distal to the subclavian artery (arrow).
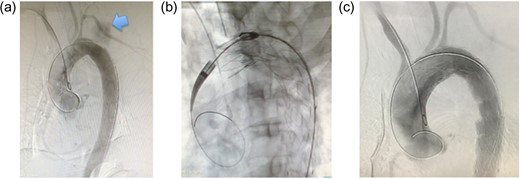
(a) Intraoperative aortography. Extravasation of contrast medium is observed (arrow). Additionally, the site of rupture could be precisely identified. (b) Intraoperative aortography. With the common femoral artery approach, stent grafts are placed between just distal to the left common carotid artery and the distal aortic arch. To achieve sufficient length of the proximal landing zone, the left subclavian artery is covered intentionally. (c) Postoperative aortography. Extravasation of contrast medium is not seen and there is no endoleak.
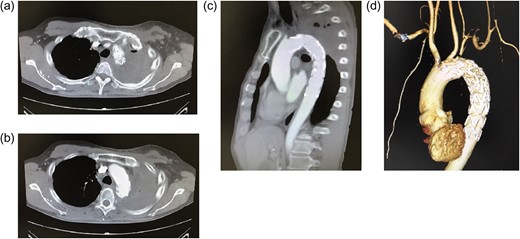
(a–c) Postoperative enhanced computed tomography (CT) (a, b: axial images; c: sagittal image). (d) 3D CT. The aortic rupture is confirmed to be effectively treated. There is no extravasation of contrast medium or endoleak. The origin of the left subclavian artery is occluded. Distal to the occluded site, the subclavian artery is perfused via collateral communications. The left vertebral artery is patent.
DISCUSSION
Aortic rupture usually occurs because of an aortic aneurysm. However, in the present case, the patient did not have an aortic aneurysm previously. In patients with lung cancer and mediastinum metastasis, direct invasion of cancer to the aorta can cause rupture. However, in our patient, progression of cancer did not occur after chemotherapy and radiation therapy, according to follow-up assessments. Additionally, the patient’s condition improved after treatment and there was no cancer recurrence. Therefore, there was no possible cause of aortic rapture, except for radiation injury. Thus, we diagnosed the patient with aortic rapture due to radiation injury at the aorta.
The patient presented with rupture 3 years after the previous radiation therapy. Radiation injury to vessels has been reported to occur even 10 years after radiation therapy [3]. Therefore, if a patient presents with aortic rapture after radiation therapy, radiation injury should be suspected, even if therapy was performed many years previously.
Radiation injury to vessels was originally described by Fajardo et al. Wolbach [4] reported the injury as ‘swelling of the endothelium and proliferation and obliteration of the capillary lumina as the cause of a roentgen ulcer’.
Stone et al. [5] reported that a large dose of radiation could cause vascular hyaline necrosis. Although elastic fibres are not feasible to radiation, a previous report mentioned that these fibres were interrupted on pathological analysis with a light microscope [6].
Tung et al. assessed radiation lesions using an electron microscope and reported irregular fragmentation of elastic fibres with non-reactive radiation necrosis in the ruptured site and slit-like space of the elastic fibre layer in radiation lesions. Lindsay et al. [7] assessed dogs who received localized aortic radiation and mentioned that atherosclerosis was strongly localized in the segment that received radiation.
A previous study suggested that micro-vessels in the vasa vasorum are occluded by radiation, which causes hypoperfusion in the elastic fibre layer, resulting in aortic perforation [8].
Operative repair is necessary for aortic rupture. The efficacy of TEVAR for thoracic aortic rupture has been reported previously [2]. In our case, TEVAR was performed for the rupture caused by radiation injury. The operation technique was not different from usual TEVAR and the procedures were straightforward.
The entry observed on preoperative enhanced CT was small, and the lesion was limited. The finding was consistent with the aetiology suggested in previous reports mentioned above.
In our case, there were few thrombi and calcifications in the proximal landing zone, and the diameter of the aorta was normal. These findings are better than the findings in patients with usual aneurysms.
We selected available grafts in the emergency setting. In order to achieve a sufficient landing zone (20 mm), we covered the left subclavian artery with a stent graft. After stent graft placement, we observed only type IV endoleak. In usual TEVAR, type IV endoleak is acceptable because it resolves spontaneously. However, in this case of aortic rupture, we decided to stop type IV endoleak immediately. Therefore, we placed another stent graft over the first one and type IV endoleak resolved.
After the operation, the haemodynamic condition stabilized. Additionally, the haemoptysis disappeared and the respiratory status stabilized. The anaemia did not progress. Moreover, the patient did not present with any complications, including paralysis. One year after the operation, the patient was well without aortic disease progression or lung cancer recurrence. These findings suggest that TEVAR for aortic rupture due to radiation injury was performed effectively. However, the long-term outcome should be assessed.
Open surgical repair is another treatment option. However, after radiation therapy, fibrosis and adhesion can occur in tissues. These changes might increase the difficulty and risk of open surgical repair. Therefore, we believe that TEVAR is more effective and safe.
In conclusion, we reported a case in which TEVAR was successfully performed for aortic rupture due to radiation injury. TEVAR is a useful treatment method for aortic rupture due to radiation injury in the aorta. Further follow-up of our patient is needed to evaluate the long-term outcomes.
ACKNOWLEDGEMENTS
Prior to the use of treatment data, consent was obtained from the patient. This report was approved by a local ethics committee (approval no. TGE 00576-025).
Consent for publication was obtained from the patient.
CONFLICT OF INTEREST STATEMENT
There is no competing interest.
REFERENCES
- anemia
- aorta
- aortic arch
- aortic diseases
- radiation therapy
- hypotension
- computed tomography
- aortic rupture
- contrast media
- back pain
- cancer
- chemotherapy regimen
- hemoptysis
- extravasation of diagnostic and therapeutic materials
- patient discharge
- pneumonia
- radiation injuries
- chest x-ray
- surgical procedures, operative
- lung cancer
- thoracic endovascular aortic repair
- recurrent lung cancer
- treatment effectiveness



