-
PDF
- Split View
-
Views
-
Cite
Cite
Ioannis D. Kostakis, Themistoklis Feretis, Paraskevas Stamopoulos, Zoe Garoufalia, Dimitrios Dimitroulis, Stylianos Kykalos, Gregory Kouraklis, Gerasimos Tsourouflis, A rare anatomical variation of the biliary tree, Journal of Surgical Case Reports, Volume 2017, Issue 5, May 2017, rjx087, https://doi.org/10.1093/jscr/rjx087
Close - Share Icon Share
Abstract
A 31-year-old woman was admitted to our department in order to undergo a laparoscopic cholecystectomy. The operation was converted to open due to cholorrhea during the dissection in the hepatocystic triangle. The cholorrhea came from a transected bile duct, which was 2 mm in diameter, came out of the hepatoduodenal ligament, ran along the common hepatic duct and drained into the cystic duct, in proximity to the neck of the gallbladder. The gallbladder was removed and an intraoperative cholangiography revealed that the aberrant bile duct was originated from the right posterior sectoral duct (RPSD). The RPSD continued its typical course up to its confluence with the right anterior sectoral duct and the formation of the right hepatic duct. This is a rare type of aberrant bile duct, which is added to the long catalogue of the anatomical variations of the biliary tree.
INTRODUCTION
The anatomy of biliary tree is complex and is characterized by the frequent presence of anatomical variations of either the intrahepatic or extrahepatic bile ducts, which can be found in ~50% of general population [1–6]. Anatomical variations of the extrahepatic bile ducts may incommode the surgeon and make the dissection in the hepatocystic triangle challenging, resulting in injuries of the extrahepatic bile ducts [1, 3, 6]. Herein, we present a case of cholecystectomy in a patient with a rare anatomical variation of the biliary tree.
CASE REPORT
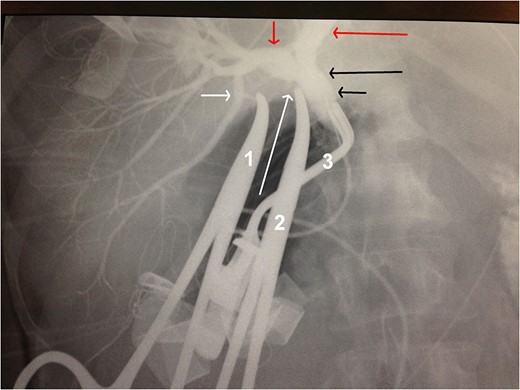
Intraoperative cholangiography. Short white arrow: the origin of the aberrant bile duct from the RPSD. Long white arrow: the stump of the cystic duct. Short red arrow: RHD. Long red arrow: LHD. Long black arrow: CHD. Short black arrow: CBD. Forceps 1 holds the stump of the aberrant bile duct. Forceps 2 holds the stump of the cystic duct. Forceps 3 blocks the CBD for the intraoperative cholangiography.
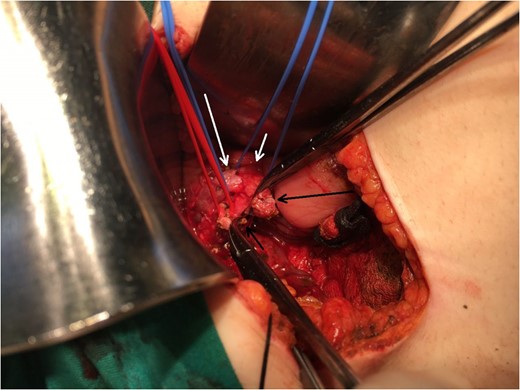
Operating field after the removal of the gallbladder. Short black arrow: the stump of the aberrant bile duct. Long black arrow: the stump of the cystic duct. Long white arrow: CHD. Short white arrow: CBD.
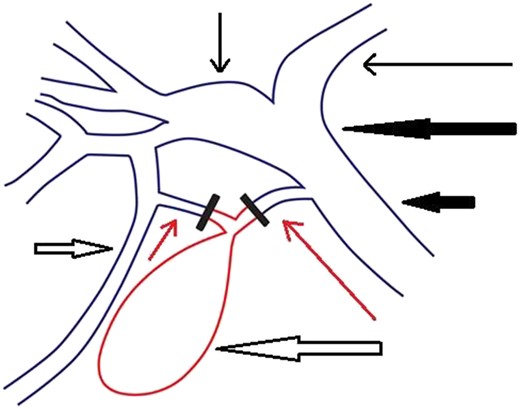
Schematic representation of the patient's biliary tree. The part of the extrahepatic biliary tree that was removed during the operation (the gallbladder, part of the cystic duct and part of the aberrant duct) is illustrated with red color. Short thin red arrow: the aberrant bile duct. Long thin red arrow: cystic duct. Long thick white arrow: gallbladder. Short thick white arrow: RPSD. Short thin black arrow: RHD. Long thin black arrow: LHD. Long thick black arrow: CHD. Short thick black arrow: CBD.
DISCUSSION
A great number of anatomical variations of the bile ducts have been reported [1–6]. Among the most common variations are the following: the draining of the RPSD into the RASD, the trifurcation of the CHD into the RPSD, the RASD and left hepatic duct (LHD), the draining of the RASD into the LHD, the draining of the RPSD into the LHD, CHD, CBD or even cystic duct, the insertion of the cystic duct into the RHD, the presence of a very short or very long cystic duct, etc. [1–6]. Furthermore, another type of variation of the biliary tree is the presence of hepaticocholecystic ducts and Luschka ducts, which connect intrahepatic ducts to the gallbaladder or its fossa [6, 7]. In our case, the RPSD joined the RASD to form the RHD, which in turn joined the LHD to form the CHD, as it is common [4, 5], but there was also an aberrant bile duct which connected the RPSD with the cystic duct. What is rare in our case is the coexistence of the common type of the RHD and CHD formation with the aforementioned type of aberrant bile duct, which is added to the long catalogue of the anatomical variations of the biliary tree. MRCP can detect the anatomical variations of intrahepatic and extrahepatic bile ducts [8]. However, as in our case, it is not routinely used prior to cholecystectomy due to its high cost and the fact that, despite the very frequent existence of anatomical variations of the biliary tree, most of them are not encountered during cholecystectomy if the surgeon dissects carefully in the hepatocystic triangle [9]. On the other hand, MRCP is very useful for the preoperative assessment of patients with suspected choledocholithiasis [10]. When the surgeon is concerned with the anatomy of the biliary tree during a cholecystectomy, an intraoperative cholangiography can be performed, as in our case, in order the biliary anatomy to be clarified and an injury to the extrahepatic bile ducts to be prevented [11]. Surgeons should always keep in mind that when they perform a cholecystectomy, either laparoscopically or open, they operate in an area with many anatomical variations and the inadvertent dissection may lead to severe bile duct injuries [1, 3, 6].
CONFLICT OF INTEREST STATEMENT
There are no conflicts of interest.
FUNDING
There is no funding regarding this article.
ETHICAL APPROVAL
No approval is required.
CONSENT
The patient gave her informed consent in order the aforementioned information to be published.



