-
PDF
- Split View
-
Views
-
Cite
Cite
Amarvir Bilkhu, Hannah Harvey, Justin B. Davies, Mark A. Steward, James C. Halstead, Laparoscopic repair of a migrated adjustable gastric band connecting tube with colonic erosion, Journal of Surgical Case Reports, Volume 2017, Issue 5, May 2017, rjx089, https://doi.org/10.1093/jscr/rjx089
Close - Share Icon Share
Abstract
Laparoscopic adjustable gastric bands are a popular and effective surgical option to treat morbid obesity. The overall complication rate is 10–20% and the most common complication is of ‘slippage’. Although other complications such as gastric band migration and erosion have been reported, the phenomenon of a migrated gastric band connecting tube eroding into the colon (after port removal) is seldom reported in the literature. In this article we describe such a case of an incidentally found colonic erosion on colonoscopy and describe the subsequent laparoscopic repair, as well as a review of the literature.
INTRODUCTION
Laparoscopic adjustable gastric bands (LAGB) are a popular and effective [1] surgical treatment for morbid obesity. Introduced in 1993 [2], the adjustable gastric band system is a surgical device that is laparoscopically placed around the stomach to create a gastric pouch (of roughly 50 mL in volume) to control caloric intake. The device consists of an inflatable band, a connecting tube and a subcutaneous port which is inflated and deflated to tighten the band around the stomach. Advantages include a minimally invasive approach, adjustability, reversibility and a quick post-operative recovery. We describe here the case of a woman where the previously divided connecting tube had migrated and eroded into the distal transverse colon.
CASE REPORT
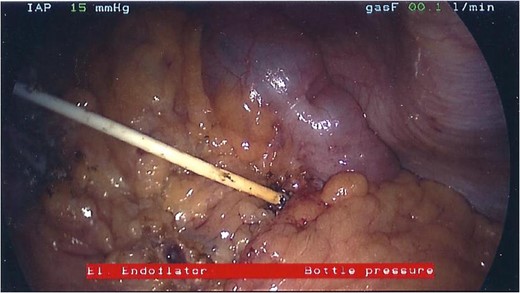
A 48-year-old female had a LAGB fitted in another institution in 2008 for obesity. She presented to our institution in December 2013 with an abscess over the port site. The abscess was drained and the port was surgically removed by dividing the port from the connecting tube. The band itself and its connecting tube were left in the abdomen at the request of the patient with an aim to reconnect the band in the future. After the patient moved location, she was lost to follow-up.

There was no evidence of sepsis and she was listed for an elective laparoscopic exploration and removal of gastric band with repair of the colon.
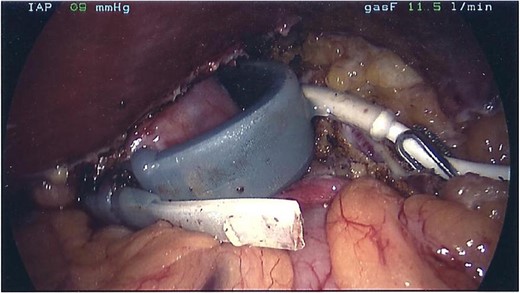
The patient was given two doses of post-operative intravenous antibiotics and kept on strictly oral fluids for 2 weeks. Her post-operative recovery was uncomplicated and she was discharged on the fourth post-operative day. Post-operative follow-up was unremarkable. Since then, she has returned to a normal diet and her usual activities of daily living.
DISCUSSION
LAGB are a popular and effective [1] surgical treatment of morbid obesity. The overall complication rate following this procedure has been reported to be up to 20% [3]. Commonly reported complications include problems with the access port (leakage, dislocation, infection and inaccessibility), pouch dilatation, prolapse or ‘slippage’ of the stomach through the band (with obstruction), balloon rupture or erosion of the band into the stomach with or without gastric necrosis. Gastric erosion of the band is a late complication seen in up to 11% [4, 5] of cases and removal can be done laparoscopically. Infection of the port area is managed by dividing the connecting tube and removal of the infected port, but this involves returning the connecting tube back into the abdominal cavity. Once sepsis has been treated and the wound healed, a new port can be attached to the connecting tube at a later date.
The migration and erosion of the gastric band into other intra-abdominal viscera is a rarer complication. There have been reports of jejunal erosion [6] but colonic erosion has only been reported four times in the literature. The first case of colonic erosion was reported in 2006 by Hartmann et al. [7] The diagnosis was made intra-operatively and the authors performed a laparoscopic procedure to remove the eroded tube from the transverse colon, repairing the colotomy with a 30 mm Endo-GIA stapling device. After reporting this complication, the authors advocate placement of a new port on the contralateral side of the upper abdomen in the same operation after removal of an infected band.
Navarra et al. [8] reported a case where the diagnosis was pre-operative (on radiography and CT imaging). They deployed a colonoscopic removal after laparoscopic dissection and division of the tube. They used a 45 mm linear laparoscopic stapler to close the colotomy. The authors advocate either securing the connecting tube to the fascia or immediate port re-siting when dealing with an infected port.
Povoa et al. [9] reported the case of a 54-year-old woman who had a gastric band placed and subsequently found to be eroded into the transverse colon on colonoscopy and CT imaging, together with simultaneous intra-gastric erosion forming a gastrocolic fistula.
Kirshtein et al. [10] reported a series of complications after gastric banding for 6382 patients fitted with a LAGB with only one case of colonic penetration, which was managed with laparoscopic exploration, band retrieval and a suture repair of the colon similar to our technique.
It has been postulated that the pathophysiology in gastric erosion is likely to stem from a port infection or progression from a gastric wall micro-perforation. Of course, division of the tube can produce a sharp tip and movements of the abdominal viscera together with respiration are also contributory.
We believe that the diagnosis of such migration and erosion should always be considered as a differential diagnosis in patients presenting with abdominal pain and sepsis with a previous history of LAGB fitting and subsequent port removal. Although the tube may have been secured to subcutaneous fascia or abdominal wall, free migration with the abdominal cavity should be assumed. Our case demonstrates that once a divided connecting tube is returned to the abdominal cavity, it should never be left for a protracted time period due to this risk of erosion into local structures. Pre-operative diagnosis and pre-operative planning should be organized with colonoscopy and radiological views on contrast-enhanced CT imaging. Treatment with a laparoscopic repair is feasible with primary closure of the colotomy with intra-corporeal interrupted mattress sutures of 3/0 PDS.
FUNDING
No financial declarations or grants.
CONFLICT OF INTEREST STATEMENT
None declared.



