-
PDF
- Split View
-
Views
-
Cite
Cite
Hiroki Sugita, Takahiko Akiyama, Naoya Daitoku, Rumiko Tashima, Hiroshi Tanaka, Shinobu Honda, Tetsumasa Arita, Yasushi Yagi, Masahiko Hirota, Internal hernia after laparoscopic right hemicolectomy, report of a case, Journal of Surgical Case Reports, Volume 2017, Issue 5, May 2017, rjw217, https://doi.org/10.1093/jscr/rjw217
Close - Share Icon Share
Abstract
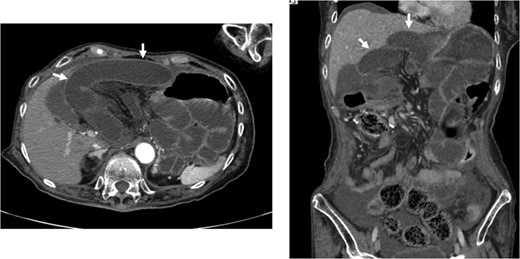
Mesenteric defects are often not closed in laparoscopic colectomy. We herein report a case of an internal hernia projecting through a mesenteric defect following laparoscopy-assisted right hemicolectomy. A 74-year-old woman was hospitalized for the surgical treatment of double colon cancer. Preoperative colonoscopy demonstrated the presence of ascending colon and transverse colon cancers. A laparoscopic-assisted right hemicolectomy was performed. The mesenteric defect resulting from the colectomy was not closed. Three months after the surgery, the patient developed a bowel obstruction. Under a diagnosis of strangulated bowel obstruction, we performed a laparotomy, and found a necrotic small bowel, which had passed into the bursa omentalis through the mesenteric defect. We removed the necrotic small bowel and closed the mesenteric defect by suturing. The patient’s postoperative course was uneventful. An internal hernia projecting through a mesenteric defect following laparoscopy-assisted right hemicolectomy developed a severe strangulated bowel obstruction.
INTRODUCTION
Laparoscopic colectomy has been accepted for benign and malignant diseases of the colon for its quicker recovery time as well as from a cosmetic viewpoint [1, 2]. In addition, long-term oncological studies have indicated that laparoscopic colectomy was equivalent to open surgery in survival rates for colon cancer [1, 3]. Therefore, laparoscopic surgery is currently the standard colon cancer treatment.
Numerous reports indicate that mesenteric defects are often not closed in laparoscopic colectomy [4]. We herein report a case of an internal hernia projecting through a mesenteric defect following laparoscopy-assisted right hemicolectomy.
CASE REPORT
A 74-year-old woman was hospitalized for the surgical treatment of double colon cancer. Her medical history showed that she had been suffering from permanent damage from a cerebral hemorrhage for several years. A colonoscopic examination demonstrated the presence of an ascending colon tumor and a transverse colon tumor. Biopsies performed before surgery revealed that both lesions were well-differentiated adenocarcinomas. A laparoscopic-assisted right hemicolectomy was performed. We divided the sub-middle colic artery and the ileocecal artery that fed the tumors with surgical trunk dissection (D3 lymph node dissection). The right colon moved out through a 5-cm midline incision. The marginal vessels were ligated, and functional end-to-end anastomosis was performed extracorporeally using linear staples. The mesenteric defect resulting from the colectomy was not closed. No herniation of the small bowel through the mesenteric defect was observed laparoscopically. Operation time was 238 min. Blood loss was 10 ml.
The double cancers were diagnosed pathologically as pT4a, pN1b, M0, pStage IIIB in the ascending colon and pT4a, pN2a, M0, pStage IIIC in the transverse colon (TNM classification seventh Edition). Capecitabine was administered as an adjuvant chemotherapy, beginning 28 days after the surgery.

DISCUSSION
With the publication of several reports demonstrating that the outcomes of laparoscopic surgery for colon cancer were equivalent to those in open surgery, this approach has become widespread in recent years [1, 3]. Laparoscopic surgery also is beneficial because of its minimal invasiveness [2].
Closure of the mesenteric defect caused by anastomosis after colectomy is not performed routinely in laparoscopic surgery [4]. Laparoscopic closure of the mesenteric defect requires a longer operation time, and incomplete closure may produce internal hernia of the small bowel. There is no consensus concerning closure of the defect. Small bowel obstructions related to mesenteric defect are rare in laparoscopic colectomy. In the case reported here, the patient developed a strangulated ileus. A narrow defect caused by mesenteric adhesion may produce the strangulation of the small bowel that passed through the mesenteric defect. The mesenterium of the colon was conglutinated to the pancreas and surgical trunk that were dissected in the first operation, resulting in the formation of a small defect of the mesenterium. Papers reported various types of internal hernias after laparoscopic colectomy [5–9]. In this case, the right hemicolectomy and the lymph nodes dissection in a wide area were necessary because of the double and advanced cancers (pT4a, pN1b, M0, pStage IIIB in ascending colon and pT4a, pN2a, M0, pStage IIIC in transverse colon). This might have allowed the tissues of the mesenterium to conglutinate more easily. Internal hernia after laparoscopic colectomy is rare. However, patients with strangulated bowel obstructions may experience severe illness. An internal hernia projecting through a mesenteric defect following laparoscopy-assisted right hemicolectomy developed a severe strangulated bowel obstruction. Therefore, a closure of the mesenteric defect may be necessary after laparoscopic colectomy.
CONFLICTS OF INTEREST STATEMENT
None declared.
REFERENCES
- cancer
- colectomy
- colonoscopy
- colorectal cancer
- synovial bursa
- hernias
- intestinal obstruction
- intestine, small
- laparoscopy
- laparotomy
- mesentery
- necrosis
- preoperative care
- surgical procedures, operative
- sutures
- diagnosis
- colon cancer
- colectomy, right
- colectomy, laparoscopic
- ascending colon
- transverse colon
- laparoscopic right hemicolectomy



