-
PDF
- Split View
-
Views
-
Cite
Cite
Ahmed Al Maksoud, Mohammed Moneer, Adel K Barsoum, Combined TRAM flap with latissimus dorsi myocutaneous flap for reconstruction of a large breast post-radiation induced necrosis, Journal of Surgical Case Reports, Volume 2017, Issue 5, May 2017, rjx079, https://doi.org/10.1093/jscr/rjx079
Close - Share Icon Share
Abstract
Radiation therapy is a critical component of breast cancer management following breast-conserving surgery. Post-radiation sequelae are greater in women with larger breasts, given the need for higher doses and dosing heterogeneity. The goal of breast reconstruction post-mastectomy is to improve the quality of life and add no more health risk. The optimal reconstruction should make the patient feel as natural as possible. Reconstruction of a large-sized breast with aesthetically satisfactory outcome poses a challenge to the breast surgeon. The breast of most Egyptian women is of a large volume with variable degrees of ptosis, thus it is difficult to reconstruct such a large-ptotic breast using an implant. We describe the successful reconstruction of a large-sized breast after radiation-induced necrosis using a combined transverse myocutaneous rectus abdominis flap and latissimus dorsi myocutaneous flap reconstruction. The combined use of both flaps offered a more natural breast reconstruction and avoided the use of any implants.
INTRODUCTION
Breast-conserving surgery (BCS) followed by whole breast radiation therapy (WBRT) is a main line of treatment for most women newly diagnosed with non-metastatic breast cancer.
Reconstruction post breast cancer surgery has gone far from simply correcting the post-mastectomy chest deformity, to restoring the form and symmetry of the breast [1].
Radiation therapy (RT) is a critical component of breast cancer management. Adjuvant RT reduces the risk of loco-regional recurrence and improves the overall survival.
CASE REPORT
A 39-year-old female who underwent a conservative surgery followed by adjuvant RT for a right breast cancer, was referred to our breast clinic with a large infected post-radiation ulcer resistant to conservative treatment for the previous year.
There was a large 15 × 20 cm2 ulcerated and infected area in the upper outer quadrant extending to the nipple and areola. The BMI of the patient was 38.3 with a large, grade 3 Regnault ptosis of the left breast.
After patient counselling, a two staged procedure was planned for reconstruction. The first stage included completion mastectomy with surgical debridement of all necrotic and infected tissues. A contra-lateral unipedicled transverse myocutaneous rectus abdominis (TRAM) flap including zones I–IV was prepared and left in place. The aim of the flap delay was to allow augmentation of the remaining blood supply and minimize the risk of infection. The residual mastectomy specimen weighted 1100 g.
During The second stage, the TRAM flap was fashioned to reconstruct the medial and lower regions of the breast. With the patient in lateral position, a pedicled latissimus dorsi myocutaneous flap (LDMF) was rotated to reconstruct the remaining defect. The abdominal wall was reconstructed using a propyl prolene mesh and the rest of the steps were completed in accordance with abdominolpasty procedure.
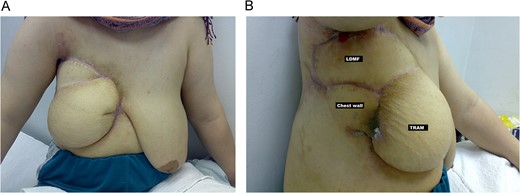
(A, frontal) and (B, lateral) Final result, 4 months post-operative, after right breast reconstruction using combined TRAM flap and LDMF.
To achieve symmetry, the patient was offered nipple reconstruction and contra-lateral mammoplasty. However, she was not keen to have any secondary procedures.
During 52 months of follow-up the patient had no flap complications and was disease free.
DISCUSSION
Breast reconstruction has proven to be a safe option that does not affect local recurrences even in locally advanced breast cancer patients. Nevertheless, it improves the patients’ quality of life and self-perception [1, 2].
The ideal breast reconstruction should offer softness, symmetry, aesthetically accepted scars, as well as texture and colour similar to the healthy breast.
The decision regarding the most appropriate reconstruction technique should take into consideration the patient’s preference, risk factors and physical characteristics [1, 3].
Increasing awareness of implant-related complications has generated high interest in reconstruction based on autologous tissue [1, 4].
TRAM flap has become the flap of choice for autologous breast reconstruction. TRAM flaps allow a more reliable transfer of large tissue, allowing for reconstruction of larger breasts than with LDMF flaps. It can be used both as pedicled or free flap [1–3].
The LDMF is one of the most reliable and versatile reconstructive methods and still the method of first choice when TRAM flaps are unavailable or unsuccessful. However, the LDMF cannot go beyond certain limits when reconstructing larger breasts and has to be combined with implants to achieve enough volume [1–3].
Reconstruction of large-sized breast with aesthetically satisfactory outcome poses a challenge to the breast surgeon. Preoperative breast size does play a role when choosing the most appropriate reconstructive option and symmetry procedure.
The breast of most Egyptian women is of a large volume with variable degrees of ptosis, thus it is difficult to reconstruct such a large-ptotic breast using an implant.
As described in this case, the combined use of both flaps offered a large volume of autologous tissue for reconstruction without the need for implants thus, improving the outcome and avoid the implant associated problems.
The deep inferior epigastric perforator uses the same lower abdominal island of skin and fat as TRAM techniques but spares the rectus abdominis muscle. However, a significant microsurgical experience is required for the meticulous dissection and anastomosis.
Secondary procedures, aiming to an as close as possible natural appearance are mostly needed. In most cases the reduction of the healthy breast side is performed to achieve symmetry. In the present case the patient was satisfied with the outcome and did not want to have any further procedures.
We describe the successful reconstruction of a large breast after radiation induced necrosis using a combined TRAM flap and LDMF. The combined use of both flaps offered a more natural reconstruction and avoided the use of any implants.
For most women treated with BCS, WBRT is recommended. Post-radiation effects are the major cause of long-term asymmetry and disfigurement, particularly in those in whom long-term survival can be expected.
Post-radiation sequelae are greater in women with larger breasts, given the need for higher doses and dosing heterogeneity. As in the current case, the radiation-induced deformities and scarring can be difficult to manage, usually requiring secondary reconstruction [5, 6].
The present case describes a young patient who underwent a complex reconstruction to manage radiation-induced resistant complication. For women with large breasts, it is important to minimize skin folds to decrease the risk of radiation-related skin toxicities. Treating these patients in a prone position can improve homogeneity and reduce other tissues exposure. The use of virtual simulation for treatment planning, compared to clinical simulation, permits a better visualization of important structures [7].
Macromastia has been considered as a relative contra-indication to BCS, due to difficulties with post-operative radiation and cosmetic outcome.
Oncoplastic surgery techniques have expanded the umbrella of BCS, and are now becoming the preferred technique. Patients with large breasts should be offered reduction mammoplasty for reconstruction as part of their BCS. Reduction mammoplasty can improve the efficacy of radiation therapy in women with large ptosed breasts [5, 6].
For women diagnosed with breast cancer, a tailored multidisciplinary approach that involves input from surgery, radiation oncology, and medical oncology is required for satisfactory outcome, both oncologically and cosmetically.
REFERENCES
- radiation therapy
- heterogeneity
- eyelid ptosis
- mammaplasty
- necrosis
- reconstructive surgical procedures
- surgical flaps
- breast
- mastectomy
- breast cancer
- breast conserving surgery
- latissimus dorsi myocutaneous flap
- rectus abdominis flap
- myocutaneous flap
- breast hypertrophy
- tram flap
- radiation necrosis
- implants



