-
PDF
- Split View
-
Views
-
Cite
Cite
Andrés Cobar, Mario Cahueque, María Bregni, Marco Altamirano, An unusual case of traumatic bilateral hip dislocation without fracture, Journal of Surgical Case Reports, Volume 2017, Issue 5, May 2017, rjw180, https://doi.org/10.1093/jscr/rjw180
Close - Share Icon Share
Abstract
Bilateral traumatic hip dislocations are extremely rare. Most of these are related to acetabular or proximal femoral fractures, consisting of complex lesions, and are rarely pure ligamentous injuries. Posterior dislocation is the most frequent. Some dislocations are accompanied by sciatic nerve palsy. The present case is a posterior bilateral hip dislocation with no other associated lesions, there are very few reports published with this clinical setting. The patient had good functional outcome.
INTRODUCTION
Traumatic isolated hip dislocation is a rare finding in an emergency room. Traumatic dislocation of the hip represents about 5% of all dislocations [1]. This injury is commonly associated with multiple lesions such as acetabular fractures, nerve palsy and femoral head fractures, due to its high energy trauma mechanism [1]. Bilateral hip dislocation is an extremely rare finding, with very few cases reported in literature [2, 3]. Most are related to acetabular or proximal femoral fractures, consisting of complex lesions, and are rarely are pure ligamentous injuries. In the diagnosis of a dislocated hip, prompt reduction must follow to prevent future complications like avascular necrosis (AVN) [1, 3].
The following case report consists in the presentation of a traumatic bilateral posterior hip dislocation without associated injuries.
CASE REPORT
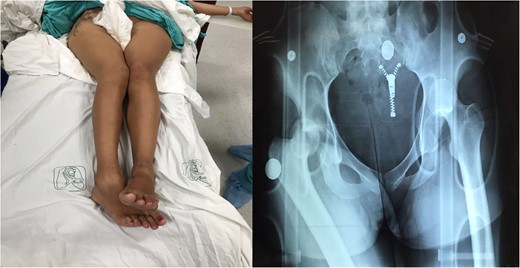
1: Patient with hip flexion and internal rotation and X-ray with traumatic bilateral posterior hip dislocation.
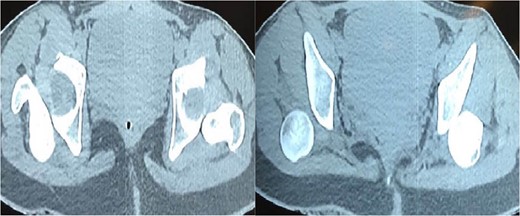
CT-Scan show bilateral posterior hip dislocation without evidence of fracture or articular fragments.

DISCUSSION
The classification of traumatic hip dislocation is based of dislocation and the degree of joint disruption including any associated joint fracture. Three commonly used classifications systems are: The Epstein classification of anterior hip dislocation [4], Pipkin sub-classification an the Thompson-Epstein Classification of posterior dislocation [5] as in this case report. Hip dislocations can be classified as simple or complex. Simple injuries are dislocations without associated fractures, whereas complex injuries include either acetabular or proximal femoral fractures [6]. Posterior dislocations represent the majority of these injuries, occurring due to an axial load of the femur, with the hip flexed and adducted. Usually, the axial load is transmitted through a flexed knee, as in dashboard injuries [3, 5, 6].
Anterior dislocations, in contrast, occur with the hip in abduction and external rotation, and the position of the femoral head can be either inferior or superior to the acetabulum. Motor vehicle accidents are the leading cause of hip dislocations, followed by falls from significant heights; sports related injuries have also been reported in literature [6, 7].
Bilateral simultaneous hip dislocations are an extremely rare injury, a reported 1.25% of all hip dislocations [3, 6–8]. These injuries are rarely present as isolated dislocations, and often associate fractures, usually of the acetabulum. These acetabular fractures frequently relate to the type of dislocation, posterior dislocation with posterior wall and column fractures and anterior dislocation with anterior wall fractures [1, 5, 7].
A patient with a dislocated hip usually presents acute pain and evident deformity, with an inability to tolerate active or passive range of motion. Of all, 95% of these patients have associated injuries, and for this reason an adequate trauma emergency evaluation must be realized in the moment of arrival, following the ATLS sequence of patient evaluation.
Pelvic x-ray films are mandatory, to detect simple or complex injuries. A CT scan is also important, presence of intra-articular fragments needs to be discarded; this imaging also functions as means of postoperative follow up [3, 7, 8]. Soft tissue injuries such as avulsions of the labrum may be assessed by magnetic resonance imaging, but are not requested routinely. Heterotopic calcifications, avascular necrosis and osteoarthritis can also be evaluated with magnetic resonance imaging as part of the patient follow up.
Treatment of hip dislocations can be either operative or nonoperative, but emergent reduction of the joint is of upmost importance. Delay in reduction of dislocated hip results in avascular necrosis in around 26% of patients [9]. Early mobilization results in a prompt return to weight bearing, but the outcome and relationship with complications such as avascular necrosis is largely debated.
Closed reduction of a posteriorly dislocated hip implies general anesthesia and an adequate positioning of the patient. Traction in line with the deformity is the principle of reduction. Several techniques have been described, all of which include traction and counter-traction as part of the maneuver [10]. Post reduction imaging studies must be performed to assess the quality of the reduction and presence of associated injuries that may have been neglected initially. Open reduction is performed in the case of an irreducible dislocation, a delayed presentation or articular fragments that make a concentric reduction impossible.
CONFLICT OF INTEREST STATEMENT
None declared.



