-
PDF
- Split View
-
Views
-
Cite
Cite
Nuttapon Arpornsujaritkun, Chairat Supsamutchai, Wiwat Thirapanich, Pitichote Hiranyatheb, Namsiri Biadul, Rare cause of massive lower gastrointestinal bleeding due to primary isolated ilio-rectal fistula, Journal of Surgical Case Reports, Volume 2017, Issue 4, April 2017, rjx074, https://doi.org/10.1093/jscr/rjx074
Close - Share Icon Share
Abstract
Massive lower gastrointestinal from primary isolated ilio-rectal fistula is a rare condition and difficult to diagnosis and emergency surgery for this situation has a high mortality rate. This report describes a successful operation in an 88-year-old man at present with massive lower gastrointestinal hemorrhage from ilio-rectal fistula and hypovolemic shock. Underlying diseases are prostate cancer, hypertension, dyslipidemia, aortic stenosis, mitral valve stenosis and chronic renal disease. Operative treatment is to explore laparotomy with internal iliac artery ligation and rectal resection. During postoperative period patient developed acute cholecystitis and treated by cholecystectomy 1 month after operation the patient went home without morbidity and 1-year follow-up he had not any complications.
INTRODUCTION
Most common cause of lower gastrointestinal hemorrhage (LGIB) in elderly patient is diverticular disease [1] and mortality rate is very low 2–4% [2]. A Massive LGIB from primary ilio-rectal fistula is rare and difficult to diagnosis but more common from secondary after previous vascular surgery. Results of ilio-rectal fistula are high morbidity and mortality [3]. A variety of treatment options are available, such as in situ graft, closure of defect alone, endovascular stent graft, extra-anatomical bypass and embolic coiling. Exploration using laparotomy for ligation internal iliac aneurysm and rectal resection is a simple operative procedure which can be applied when emergency option is needed to save a life. We describe successful emergency surgery in primary ilio-rectal fistula when patient presents a massive LGIB and hypovolemic shock.
CASE REPORT
An 88-year-old man, his underlying diseases are hypertension, dyslipidemia, moderate aortic stenosis and mitral valve stenosis, chronic kidney disease and prostate cancer. He developed massive rectal bleeding with syncope 1 hour before visiting the hospital.
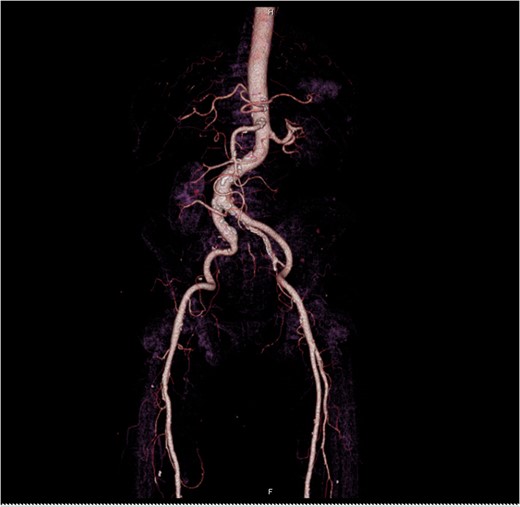
At Emergency department, physical exam showed hypotension blood pressure 70/50 mmHg and per rectal exam showed blood clot with enlarged prostate. After resuscitation until stable vital sign, he was sent for colonoscopy but cannot be evaluated due to a lot of blood clots in the rectum. He was admitted for observation and we planned to repeat colonoscopy again following day because he was stable and bleeding was stopped. Following day after admitting, he had massive lower gastrointestinal bleeding again fresh blood ~1000 ml from his anus. His blood pressure was lower 80/50 mmHg. After stabilization, we planned to send the patient to angiogram for embolization. But the patient had a problem vascular access site and then send to computed tomography angiography (CTA) for evaluate access site. We found 3 cm aneurysm of right internal iliac artery with partial thrombus and attached to rectosigmoid colon with leakage of contrast into sigmoid lumen (Figs 1–2). He was sent to operating room during transferring we gave blood transfusion and then emergency explore laparotomy was performed, the operation performed by partial aneurysmectomy, ligated right internal iliac, wedge resection rectum wall and temporary abdominal closure with swab packing due to bowel distension and abdominal pressure was high. The operative time was around 3 hours and blood loss 6000 cc. He was sent to operating room for change swab packing on Day 3 and permanent abdominal closure on Day 5. During postoperative period, he developed acute cholecystitis and underwent open cholecystectomy. After admit for 1 month, he was discharged with fully recovery.
DISCUSSION
Primary aorto/ilio-enteric fistula (PAEF) is very rare, but secondary fistula is more common. Sir Astley Cooper was the first to describe a PAEF as a condition caused by spontaneous erosion of the aorta into the gastrointestinal tract. Incidence of PAEF ~0.07% in the general population from large autopsy series [4]. Etiology of PAEF are several causes, most causes are due to aneurysm, infection, tumor, radiotherapy and foreign body ingestion [5–9]. The most common site of fistula located in duodenum 54%, esophagus 28%, small bowel and large bowel 15% [9]. The classical triad of symptoms associated with a fistula is gastrointestinal hemorrhage, abdominal pain and a pulsating abdominal mass. Most common sign and symptoms of fistula is gastrointestinal bleeding, but only 11% presented with classical triad [9].
The diagnosis of PAEF is difficult to make. Because most of patients were send to endoscope due to gastrointestinal bleeding symptoms. Endoscope frequently fail to diagnosis because of a lot of blood. Several diagnosis investigations were used when patients are clinically stable such as CTA, angiography, colonoscopy, and red blood cell scan. All of these do not constitute specific investigation. However, CT scan can diagnose specifically aorto/ilio-enteric fistula (for example, air within aortic wall or contrast fill in bowel lumen) that detection rate 61% when failure diagnosis from endoscopy [9].
There are several treatment options for PAEF. Such as, in situ graft, closure of defect alone, endovascular stent graft, extra-anatomical bypass and embolic coiling. Optional treatment depends on surgeon’s experience, hospital facilities and the type of PAEF. The overall mortality rate of PAEF after treatment is 44% [9].
This case was send to the operating room after diagnosis right internal ilio-rectal fistula for emergency exploration with laparotomy because the patient’s active bleeding and vital signs were not stable preventing adequate preparation time for intervention or stent graft in hospital. We decided to ligate right internal iliac artery, wedge resection rectum with suture repair because this is a simple operation and can save patient’s life. Other options could be done by endovascular therapy or embolic coiling if we had time to prepare and the patient was already stabilized in this hospital.

Axial view iliac aneurysm with partially thrombose contact rectosigmoid colon and contrast leak.

CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- aortic valve stenosis
- dyslipidemias
- cholecystitis, acute
- hypertension
- mitral valve stenosis
- kidney failure, chronic
- cholecystectomy
- pathologic fistula
- follow-up
- hypovolemic shock
- laparotomy
- diagnosis
- morbidity
- mortality
- lower gastrointestinal bleeding
- prostate cancer
- internal iliac artery ligation
- rectum excision
- emergency surgical procedure



