-
PDF
- Split View
-
Views
-
Cite
Cite
Eline A. Caine, Thomas H. Newman, Omar Marzouk, Kathryn Lynes, Mansoor Akhtar, Subacute bowel obstruction secondary to an obturator hernia: case report and a review of the literature, Journal of Surgical Case Reports, Volume 2017, Issue 4, April 2017, rjx061, https://doi.org/10.1093/jscr/rjx061
Close - Share Icon Share
Abstract
Obturator hernias are rare and are often diagnosed late. This case report discusses an 82-year-old female who had symptoms of subacute bowel obstruction. Following a computed tomography abdomen pelvis, she underwent a laparotomy for an incarcerated right obturator hernia. The hernia was repaired using a single suture and she made a good recovery. A review of the literature around obturator hernias is discussed.
INTRODUCTION
Obturator hernias account for only 1% of all intra-abdominal hernias [1]. Despite this, they still are associated with high mortality [2]. Obturator hernias often present as small bowel obstruction [3] and even then these symptoms can be non-specific. Our case reports describes these non-specific symptoms in an 82-year-old female and how imaging aided a difficult diagnosis. High suspicion for obturator hernias may lead to earlier surgical management; both open and laparoscopic techniques are used.
CASE REPORT
An 82-year-old female was admitted to a district general hospital overnight with right iliac fossa and central abdominal pain. She had vomited once and last opened her bowels 2 days earlier, although she was passing flatus.
She had no change in bowel habit or weight loss during the preceding weeks or months. She lived alone, was independent and her past medical history included gastro-oesophageal reflux disease and oesophagitis. She had no significant past surgical history.
She was admitted earlier in the year with similar symptoms under medical physicians, and discharged on resolution of symptoms. However, on reviewing her notes, it was noted that a computed tomography abdomen pelvis (CTAP) at that time indicated a possibility of obturator hernia.
During this admission her examination revealed tenderness over the right femoral triangle, but no palpable lumps or hernias were noted. Per rectal examination was unremarkable. Her observations were within normal limits, blood tests were unremarkable and an arterial blood gas demonstrated a lactate of 1.0 mmol/L. Abdominal plain radiograph showed faecal loading and chest plain radiograph did not show free air under the diaphragm. She was admitted with a nasogastric tube, IV fluids, analgesia and kept nil by mouth. A CTAP was requested following consultant review in the morning.
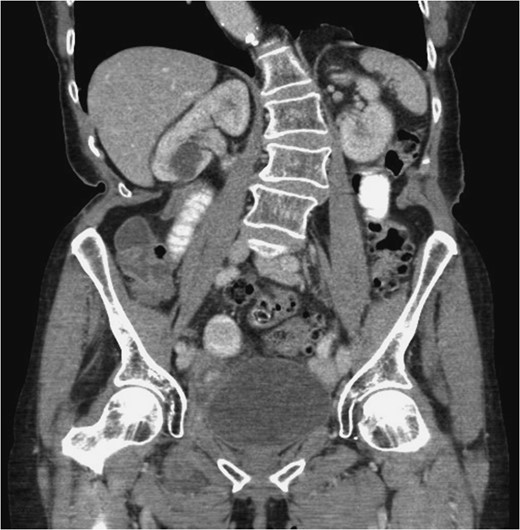
Coronal plane. The right obturator hernia is demonstrated. It contains small bowel loop. Proximal small bowel is mildly dilated. Right obturator hernia with features of incomplete small bowel obstruction.


Segment of incarcerated bowel after release from hernia defect.
Post-operative period was uneventful and she made a good recovery.
DISCUSSION
Obturator hernias are sometimes referred to as ‘little old lady’s hernia’, typically affecting elderly thin women. This is thought to be due to the fact that women have wider pelvises, larger obturator canals and atrophy or loss of pre-peritoneal fat around the obturator vessels predisposing to hernia formation [2, 3].
Obturator hernias are extremely rare accounting for ~1% of all intra-abdominal hernias [1]. Despite this they are still associated with a high mortality rate [2]. This may be attributed to the fact that they are difficult to diagnose clinically as signs and symptoms may be non-specific [4]. In fact, most (88%) obturator hernias have been diagnosed when presenting as small bowel obstruction [3] and even then symptoms may be intermittent. Patients may also present with a palpable mass in the groin identified when the patient is supine with hip flexed and laterally rotated [5]. Other presentations may include pain on the medial aspect of the thigh on extension, adduction or medial rotation of the hip (Howship–Romberg sign) or loss of adductor reflex (Hannington-Kiff sign) on examination [4]. Given the difficulty in diagnosing obturator hernias, CT is the choice of imaging for diagnosis.
Surgical intervention is the definitive management of an obturator hernia causing small bowel obstruction; both laparoscopic and open techniques have been demonstrated. In cases of emergency admission with small bowel obstruction the standard operation would be a laparotomy with an infraumbilical midline incision, but there may be occasions when laparoscopy could be considered. There have been a few published case series in selected situations suggesting that laparoscopic repair can be used in the acute setting with incarcerated obturator hernias [6–9]. If the bowel is suspected to be ischaemic on CT a laparotomy is favoured [6], the advantage being that the site of obstruction can be quickly identified and managed [2].
In our case we used simple sutures, which have been shown to be effective and safe when closing the hernial defect for obturator hernias [2].
Some recent case series have shown that a laparoscopic two-step approach can be taken in patients who have incarcerated hernias requiring bowel resection. One study initially used a laparoscopic bowel resection followed by a totally extra-peritoneal mesh repair 9 days later [9]. Another study used a transabdominal pre-peritoneal repair as the second step following initial laparoscopic bowel resection [10].
CONCLUSION
In summary, our patient had the typical characteristics of a patient with an incarcerated hernia; female, elderly and thin. This case highlights the difficulty in diagnosing obturator hernias, particularly as she presented with similar symptoms earlier in the year. Obturator hernias are rare, and there is much less in the literature in comparison to other hernias. There are a limited number of studies with selective criteria describing laparoscopic repair of obturator hernia in the emergency setting. Lower midline infraumbilical laparotomy is a safe and quick method to identify and repair an obturator hernia without complication. A laparotomy additionally allows inspection of the bowel for viability.
ACKNOWLEDGEMENTS
Eline A. Caine: Carried out the background research, wrote the draft and formatted the report.
Thomas H. Newman: Reviewed and edited the draft.
Omar Marzouk: Instigated the work by presenting the case as a powerpoint presentation.
Kathryn Lynes: Reviewed the final draft.
Mansoor Akhtar: Consultant surgeon who performed the operation. Oversaw the writing and editing of the report.
CONFLICT OF INTEREST STATEMENT
None declared.



