-
PDF
- Split View
-
Views
-
Cite
Cite
Andrea Carollo, Travis Rosenkranz, D. James Smith, Cancer of unknown primary (CUP) presenting as a Spigelian hernia: a case report, Journal of Surgical Case Reports, Volume 2017, Issue 4, April 2017, rjw218, https://doi.org/10.1093/jscr/rjw218
Close - Share Icon Share
Abstract
Cancer of unknown primary (CUP) is a well-known entity that can present in a multitude of clinical presentations. Based on the extent and organ of involvement, the presentation will be varied. For instance, patients presenting with axillary lymphadenopathy would lead toward a primary breast cancer, whereas patients presenting with abdominal distention due to ascites would tend toward a gastrointestinal origin. We present a case of a 73-year-old female who presented with an abdominal wall mass; on laparoscopy, she was found to have a spigelian hernia due to an omental metastatic lesion from a CUP.
INTRODUCTION
Cancer of unknown primary (CUP) is a well-recognized clinical disorder, accounting for 3–5% of all malignant epithelial tumors [1]. It is characterized as an aggressive disease with an early dissemination of metastases without a primary detected site after extensive laboratory and clinical investigations [2]. The National Comprehensive Cancer Network (NCCN) have set forth guideline for work-up based on clinical presentation, with all including extensive history and physical exam, computed tomography (CT) of chest/abdomen/pelvis and site/gender-specific diagnostic studies (i.e. mammogram and testicular US) and tumor markers (i.e. CA-125 and prostate specific antigen [PSA]), as well as appropriate immunohistochemistry.
CASE REPORT
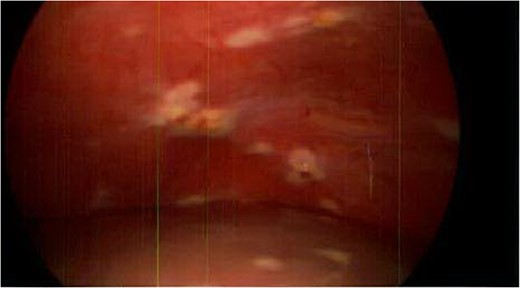


Spigelian hernia. Omental metastatic lesion protruding through the semilunar line.
DISCUSSION
CUP is divided into two subsets, favorable (20%) and unfavorable (80%), based on histopathology and clinical presentation (Table 1). About 80% of cases that are first diagnosed as CUP eventually have a confirmed type. Roughly 60% of CUP primary sites are adenocarcinomas arising from glandular cells (lung, pancreas, breast, prostate, stomach, colon and liver) while the remaining sites of origin include melanoma, sarcoma, lymphoma and neuroendocrine tumors [3]. Patient presentation varies depending on the location of metastasis. Common presentations are non-specific such as non-tender swollen lymph nodes, palpable mass in the abdomen, pain in the bones and unexplained weight loss. Patients with carcinoma of unknown primary site are heterogeneous with respect to tumor biology, clinical characteristics and response to therapy. Extensive work-up with specific pathology investigations (immunohistochemistry, electron microscopy, molecular diagnosis) and modern imaging technology (CT, mammography and PET scan) have resulted in some improvements in diagnosis; however, the primary site remains unknown in most patients, even on autopsy [4]. Subsequent evaluation and treatment differ depending on the classification of CUP. In our case, the patient has a mixed favorable and unfavorable profile since she has a cancer that closely resembles a colonic origin, but presented with liver metastasis.
| Favorable subsets . | Unfavorable subsets . |
|---|---|
| 1.Women with adenocarcinoma involving axillary lymph nodes | 1. Adenocarcinoma metastatic to the liver or other organs |
| 2. Women with papillary carcinoma involving the peritoneal cavity | 2. Poorly differentiated carcinoma |
| 3. Squamous cell carcinoma involving cervical lymph nodes | 3. Non-papillary malignant ascites (adenocarcinoma) |
| 4. Poorly differentiated neuroendocrine carcinomas. Merkel cell carcinoma of unknown primary (localized disease) | 4. Multiple cerebral metastasis (adeno or squamous carcinoma) |
| 5. Adenocarcinoma with a colon profile (CK20+, CK7−, CDX2+) | 5. Multiple lung/pleural metastasis (adenocarcinoma) |
| 6. Isolated inguinal adenopathy (squamous carcinoma) | 6. Multiple metastatic bone disease (adenocarcinoma) |
| 7. Men with blastic bone metastasis and elevated PSA (adenocarcinoma) | 7. Squamous cell carcinoma of the abdominal cavity |
| 8. Patients with a single, small, potentially resectable tumor |
| Favorable subsets . | Unfavorable subsets . |
|---|---|
| 1.Women with adenocarcinoma involving axillary lymph nodes | 1. Adenocarcinoma metastatic to the liver or other organs |
| 2. Women with papillary carcinoma involving the peritoneal cavity | 2. Poorly differentiated carcinoma |
| 3. Squamous cell carcinoma involving cervical lymph nodes | 3. Non-papillary malignant ascites (adenocarcinoma) |
| 4. Poorly differentiated neuroendocrine carcinomas. Merkel cell carcinoma of unknown primary (localized disease) | 4. Multiple cerebral metastasis (adeno or squamous carcinoma) |
| 5. Adenocarcinoma with a colon profile (CK20+, CK7−, CDX2+) | 5. Multiple lung/pleural metastasis (adenocarcinoma) |
| 6. Isolated inguinal adenopathy (squamous carcinoma) | 6. Multiple metastatic bone disease (adenocarcinoma) |
| 7. Men with blastic bone metastasis and elevated PSA (adenocarcinoma) | 7. Squamous cell carcinoma of the abdominal cavity |
| 8. Patients with a single, small, potentially resectable tumor |
| Favorable subsets . | Unfavorable subsets . |
|---|---|
| 1.Women with adenocarcinoma involving axillary lymph nodes | 1. Adenocarcinoma metastatic to the liver or other organs |
| 2. Women with papillary carcinoma involving the peritoneal cavity | 2. Poorly differentiated carcinoma |
| 3. Squamous cell carcinoma involving cervical lymph nodes | 3. Non-papillary malignant ascites (adenocarcinoma) |
| 4. Poorly differentiated neuroendocrine carcinomas. Merkel cell carcinoma of unknown primary (localized disease) | 4. Multiple cerebral metastasis (adeno or squamous carcinoma) |
| 5. Adenocarcinoma with a colon profile (CK20+, CK7−, CDX2+) | 5. Multiple lung/pleural metastasis (adenocarcinoma) |
| 6. Isolated inguinal adenopathy (squamous carcinoma) | 6. Multiple metastatic bone disease (adenocarcinoma) |
| 7. Men with blastic bone metastasis and elevated PSA (adenocarcinoma) | 7. Squamous cell carcinoma of the abdominal cavity |
| 8. Patients with a single, small, potentially resectable tumor |
| Favorable subsets . | Unfavorable subsets . |
|---|---|
| 1.Women with adenocarcinoma involving axillary lymph nodes | 1. Adenocarcinoma metastatic to the liver or other organs |
| 2. Women with papillary carcinoma involving the peritoneal cavity | 2. Poorly differentiated carcinoma |
| 3. Squamous cell carcinoma involving cervical lymph nodes | 3. Non-papillary malignant ascites (adenocarcinoma) |
| 4. Poorly differentiated neuroendocrine carcinomas. Merkel cell carcinoma of unknown primary (localized disease) | 4. Multiple cerebral metastasis (adeno or squamous carcinoma) |
| 5. Adenocarcinoma with a colon profile (CK20+, CK7−, CDX2+) | 5. Multiple lung/pleural metastasis (adenocarcinoma) |
| 6. Isolated inguinal adenopathy (squamous carcinoma) | 6. Multiple metastatic bone disease (adenocarcinoma) |
| 7. Men with blastic bone metastasis and elevated PSA (adenocarcinoma) | 7. Squamous cell carcinoma of the abdominal cavity |
| 8. Patients with a single, small, potentially resectable tumor |
CUP is a clinical entity that is not as uncommon as previously thought. As our patients’ CUP presented as a spigelian hernia this is quite a rare occurrence. Spigelian hernias are anterior abdominal wall hernias that occur at a defect adjacent to the semilunar line and they comprise only 0.12% of all abdominal wall hernias and are difficult to diagnose clinically depending on its location [5]. Though rare concomitant disease processes, CUP as a spigelian hernia should be included in the differential diagnosis of anterior abdominal wall masses, even in the absence of symptoms suggestive of cancer.
CONFLICT OF INTEREST STATEMENT
None declared.



