-
PDF
- Split View
-
Views
-
Cite
Cite
Lawrence Hayes, Charlotte Newton, Gastric outlet obstruction secondary to caecal herniation into the lesser sac, Journal of Surgical Case Reports, Volume 2017, Issue 4, April 2017, rjx076, https://doi.org/10.1093/jscr/rjx076
Close - Share Icon Share
Abstract
Internal hernias comprise 1% of hernias, 8% of which are through the foramen of Winslow into the lesser sac. These hernias can mimic gastric outlet obstruction and cause associated morbidity. In this case, we describe a caecal herniation into the lesser sac presenting as true gastric outlet obstruction in a 69-year-old female. Initial computed tomography (CT) imaging demonstrated a distended stomach with collapsed small bowel representing likely gastric outlet obstruction. Nasogastric tube insertion decompressed the stomach but the clinical picture progressed to that of small bowel obstruction with generalized abdominal distension and hypoactive bowel sounds. Repeat CT demonstrated caecal herniation into the lesser sac. This was confirmed at exploratory laparotomy with the caecum found in the lesser sac via the foramen of Winslow. The caecum was grossly ischaemic with patchy necrosis. A limited right hemicolectomy was performed. The patient made an uncomplicated recovery and was discharged on the eighth post-operative day.
INTRODUCTION
Internal hernias comprise 1% of hernias, 8% of which are through the foramen of Winslow into the lesser sac. These hernias can mimic gastric outlet obstruction and cause associated morbidity.
This is the third reported case describing true gastric outlet obstruction secondary to caecal herniation through the lesser foramen. It is common for this type of herniation to initially be misinterpreted as a gastric outlet obstruction. In this case, we observed a temporal progression from the treated gastric outlet obstruction to ongoing bowel obstruction caused by caecal herniation into the lesser sac.
CASE REPORT
A 69-year-old female presented with a 1-day history of acute onset left upper quadrant (LUQ) pain. The pain radiated around the upper abdomen and was associated with nausea and retching. She had normal bowel opening at presentation and described feeling sweaty and cold on systems enquiry. She had a previous history of hypertension and hysterectomy.
On examination, she was severely tender with a localized 15×15 cm smooth, tympanic mass in the LUQ, otherwise the abdomen was soft and non-tender with normal bowel sounds (BS). Clinically, she was in atrial fibrillation with fast ventricular response (AF) at a rate of 170 bpm with BP 180/100. All other observations were normal.
Computed tomography (CT) imaging demonstrated gastric outlet obstruction with collapsed small bowel loops, initially interpreted as possible gastric duplication cyst.
Management with nasogastric (NG) tube decompressed the stomach but she remained in refractory fast AF despite metoprolol and amiodarone loading. Upper GI endoscopy demonstrated fundal and proximal body congestion with uninterrupted scope passage into the duodenum. High NG tube aspirates continued despite resolution of the large LUQ mass, and she developed generalized abdominal distension with hypoactive BS. Repeat CT scan demonstrated caecal herniation into the lesser sac and distended loops of obstructed small bowel, with normal appearances of the stomach. The patient proceeded to exploratory laparotomy, which found small bowel obstruction caused by caecal volvulus and herniation through the foramen of Winslow. The caecum was ischaemic and non-viable with patches of necrosis. The caecum was decompressed in the lesser sac via the appendiceal orifice and a limited right hemicolectomy performed with primary anastomosis. The patient was transferred to the ITU. She made a steady and uncomplicated recovery to discharge on the eighth post-operative day.
DISCUSSION
Internal hernias are uncommon comprising 1% of all hernias [1], of these ~8% are into the lesser sac [2, 3], with paraduodenal (53%), pericaecal (13%) and transmesenteric (8%) forming the majority of other internal hernias. There are nearly 150 cases of hernia into the lesser sac described in the literature [4]. Of these, small bowel (60%) and ascending colon (25–30%) are the most common [2].
This is the third reported case to describe gastric outlet obstruction in the context of herniation through the lesser foramen [5], and herniation through the hepatogastric ligament [6]. We feel this case is unique as it provides insight into the temporal progression of these presentations, from both a clinical and radiological perspective.
A common clinical presentation is that of obstruction with abdominal distension, epigastric pain, nausea and vomiting. Patients may describe curling into a ball or leaning forward as a relieving factor, which corresponds with an increase in size of the opening into the lesser sac lessening pressure on the obstructed viscus [7].
Owing to the presentation often mimicking gastric outlet obstruction, imaging is the only reliable pre-surgical diagnostic investigation. Commonly employed modalities include plain film, upper GI contrast studies and CT. Several authors have described characteristic X-ray findings that can aide identification, but CT remains the modality of choice owing to speed and reconstruction capabilities [8]. In this case, we proceeded straight to CT, based on the likely complexity of the intra-abdominal pathology. Characteristic CT findings described by Patel and Newton [9] can be retrospectively applied to this case: air-fluid levels in the lesser sac with distended bowel loops in the sub-hepatic space and absence of ascending colon in its normal anatomical position.
Once diagnosis has been established prompt surgical management is essential with mortality approaching 50% even with treatment, excess mortality has been attributed to delays in instigating surgical management [10]. In this case, we proceeded to laparotomy, but an alternative approach is with minimally invasive surgery.
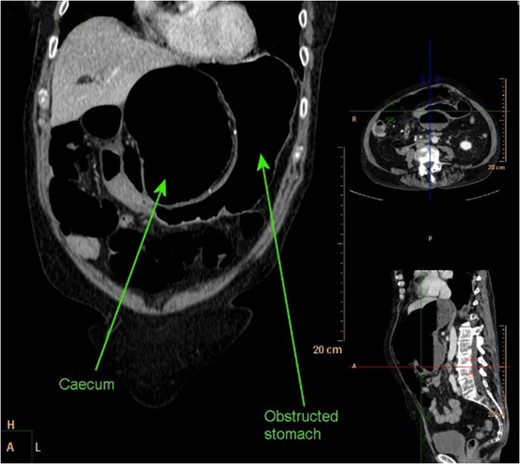
CT abdomen coronal reconstruction demonstrating obstructed stomach with obstructed and dilated caecum present in lesser sac.
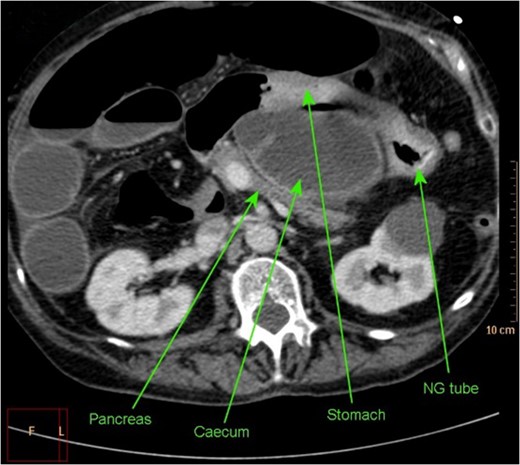
Axial section of CT abdomen demonstrating NG tube in stomach, with successful decompression of obstructed gastric outlet, however obstructed caecum clearly visible within lesser sac.
CONFLICT OF INTEREST STATEMENT
None declared.
PATIENT CONSENT TO PUBLICATION
Written informed consent was obtained from the patient for publication of this case report and accompanying images. Copies of the written consent are available for review by the Editor-in-Chief of this journal on request.



