-
PDF
- Split View
-
Views
-
Cite
Cite
Stephen Kunz, Su Kah Goh, Wanda Stelmach, Siven Seevanayagam, Traumatic rupture of the diaphragm resulting in the sub-acute presentation of an incarcerated intra-thoracic transverse colon, Journal of Surgical Case Reports, Volume 2017, Issue 3, March 2017, rjx057, https://doi.org/10.1093/jscr/rjx057
Close - Share Icon Share
Abstract
The traumatic rupture of the diaphragm after blunt or penetrating injuries is a well described but uncommon entity. Its presentation in the form of herniated abdominal contents into the thoracic cavity is generally obscure and the recognition of this condition is often challenging. Although many cases remain asymptomatic, significant morbidity and mortality ensues with patients who present with incarceration, strangulation and eventual visceral compromise. Definitive guidelines in the management of traumatic diaphragmatic injuries are still lacking. This report outlines a case of sub-acute presentation of a traumatic diaphragmatic rupture in an elderly female following a motor vehicle accident that required urgent surgical intervention. We reviewed the pertinent literature, with an emphasis on the operative approach and the type of repair of the traumatic diaphragmatic defect.
INTRODUCTION
Traumatic diaphragmatic injury (TDI) is an uncommon and potentially life-threatening clinical entity, occurring in 0.47–5% of cases of thoracoabdominal injuries [1–3]. They can present in acute, latent, or obstructive phases, and may occur at the initial injury to many years later [3]. Due to the non-specific presenting symptomatology, the diagnosis of TDI is challenging and requires a high index of suspicion.
Acute herniation, presenting in up to 70% of cases, occurs due to sheer forces within the abdomen from high-velocity injury causing disruption of the diaphragm's peripheral attachments, creating a defect. As a result of the subsequent thoracoabdominal pressure gradient colonic, omental, gastric, splenic, hepatic and renal herniation have been described, with the majority (80%) being located on the left side of the diaphragm [3, 4]. This herniation can manifest as chest pain, regurgitation, dysphagia, dyspnoea, nausea/vomiting or abdominal pain, or in up to 50% of patients, asymptomatically [1, 5]. As a result, only 43.5% of cases of TDI are diagnosed pre-operatively [4].
Latent herniation is thought to be a combination of this initial tear, compounded by devascularisation, thinning and necrosis of the diaphragm. The defect may cause transient herniation, or can develop into incarceration, strangulation or rupture. It shares the range and non-specificity of symptoms with those of acute presentation [4].
Finally, the obstructive phase manifests as compromise of the herniated viscera, most commonly the transverse colon, and carries up to an 80% mortality, illustrating the need for a low threshold for investigation of individuals with prior significant mechanism [3]. Despite limited guidelines in the management of TDI, the recognized significant morbidity and mortality has led to many surgeons performing an acute repair [5].
The purpose of this report is to highlight the case of a patient presenting sub-acutely, with a TDI and incarcerated bowel following a motor vehicle accident. The operative decisions undertaken are discussed in relation to the current literature.
CASE REPORT
A healthy 61-year-old woman presented following a single vehicle accident collision with a tree at 50 km/h. Primary and secondary survey revealed a small left pneumothorax (~10%), multiple left rib fractures, a deep laceration to her left knee and a closed displaced fracture of her right head of humerus. Her respiratory status was stable. Her pneumothorax was initially managed conservatively. The soft tissue and orthopaedic injuries were managed operatively under spinal anaesthesia. Due to the persistence of the pneumothorax, an intercostal catheter was placed on Day 3. She remained clinically well.
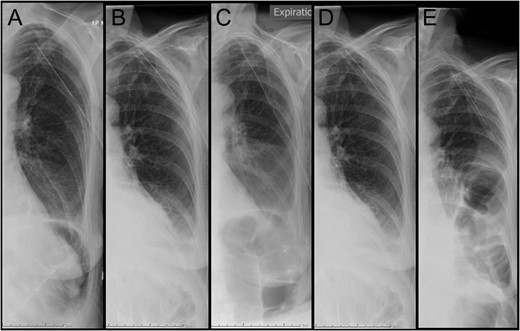
Daily chest x-ray documenting the left hemithorax. (A) Day 3 post admission: immediately post insertion of intercostal catheter. (B–D) consecutive chest x-ray on Days 4, 5 and 6 post admission. (E) Day 7 post admission: diagnostic of bowel loops in left hemithorax.

Representative coronal slice of computed tomography confirming the presence of a traumatic diaphragmatic hernia with a loop of incarcerated colon in the left hemithorax.
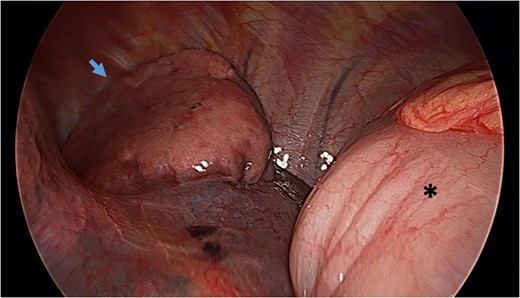
Video-assisted thoracoscopy (VAT) demonstrating a loop of transverse colon in the left hemithorax. Black asterisk (*) indicates a loop of transverse colon. Blue arrow indicates deflated left lung.
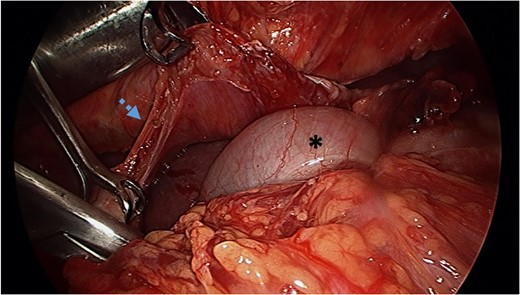
Reduction of transverse colon into abdominal cavity. The spleen is visible adjacent to the transverse colon. Black asterisk (*) indicates a loop of transverse colon. Blue broken arrow indicates the diaphragmatic defect that was extended to successfully reduce the colon.
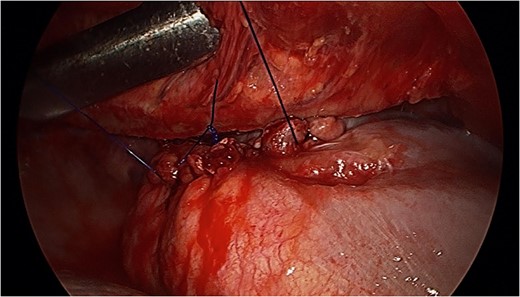
Tension-free primary suture repair of the diaphragmatic defect.
Her post-operative imaging was satisfactory, her recovery uneventful, and she was discharged Day 5 post-operatively. She has since remained well.
DISCUSSION
This case highlights an asymptomatic case of a traumatic diaphragmatic hernia 7 days following blunt trauma. The risk of strangulation of the incarcerated transverse colon prompted the need for urgent surgical intervention. The operative approach and the type of repair undertaken in this case facilitated the positive outcome for this patient.
Approaches
Once the diagnosis has been achieved, operative intervention can be performed through the chest, abdomen, or thoracoabdomen.
One review of the literature revealed that 74% of patients with TDI had their injuries repaired via laparotomy, 18% via thoracotomy and 8% had thoracoabdominal approaches [6]. A later cohort study showed 9% of patients underwent laparoscopy [7], and some centres advocate for VATS repair [8, 9].
Due to the potential for concomitant abdominal injuries [2], an abdominal approach allows for diagnosis of visceral injuries needing repair or resection, however, right-sided diaphragmatic hernias can be difficult to repair due to the need for hepatic mobilization [5, 6]. By contrast a thoracic approach allows for a greater sensitivity in detecting occult diaphragmatic injuries and associated chest injuries, however, it precludes thorough assessment of additional abdominal trauma, and thoracotomies are associated with the longest post-operative recovery time [7]. While there are no randomized controlled trials comparing outcomes between abdominal and thoracic approaches, or open and minimally invasive repairs, current literature recommends that the operative decisions be guided by the experience of the institution and operating surgeon [6, 9, 10].
Given that our patient was one week post-trauma, without any clinical or radiological evidence of additional injuries, our decision was to trial a VATS approach, with the rationale being this would allow minimally invasive assessment of the herniated colon's integrity and division of any intra-thoracic adhesions. Although the thoracoscopic repair was unsuccessful, the direct visualization of the defect allowed for a smaller thoracotomy to be made, and our patient's post-operative length of stay was comparable with that of laparoscopic intervention seen in other series [9].
Upon reduction of the hernia, balancing the risks of recurrence and infection between primary or mesh repairs can be challenging. There is a paucity of literature to determine whether primary or mesh repair is most appropriate. Given our patient's presentation, juxtaposed with the intra-operative findings of healthy diaphragm but intra-pleural free fluid, a tension-free primary repair using a non-absorbable suture was deemed appropriate.
LEARNING POINTS
– TDI is uncommon and its diagnosis challenging
– It should be suspected in cases of blunt thoracoabdominal trauma
– Visceral compromise is associated with significant morbidity and mortality
– Abdominal access is useful to assess for concomitant visceral injury
– Thoracic access is useful in delayed presentations, and in right-sided trauma.
REFERENCES
Author notes
Co-first author.



