-
PDF
- Split View
-
Views
-
Cite
Cite
Aysha N. Khan, Jesse T. Casaubon, John Paul Regan, Leonora Monroe, Cocaine-induced splenic rupture, Journal of Surgical Case Reports, Volume 2017, Issue 3, March 2017, rjx054, https://doi.org/10.1093/jscr/rjx054
Close - Share Icon Share
Abstract
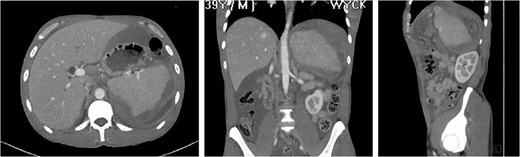
Splenic rupture is a rare but serious complication from cocaine abuse. Given the ubiquitous prevalence of abuse and the potential for death from intraperitoneal bleeding, the prompt diagnosis and treatment of cocaine-induced disease including splenic rupture is essential. The management for splenic rupture from traumatic and atraumatic etiology has shifted from emergent laparotomy and splenectomy to non-operative approach with transcatheter splenic artery embolization. We report a 39-year-old male with a significant substance abuse history who presented with atraumatic splenic rupture. He was managed nonoperatively with adjunctive transcatheter splenic artery embolization. His post-procedure course was complicated by an intra-abdominal abscess requiring drainage via interventional radiology guided pigtail catheter placement and intravenous antibiotics. This case report is intended to raise awareness of the potentiating effects of cocaine use in this patient population and highlight questions raised during this patient's management.
INTRODUCTION
Cocaine is a potent stimulant of the central nervous system which causes vasoconstriction and can damage all organ systems [1]. It blocks presynaptic sympathetic reuptake of norepinephrine (NE), causing accumulation in synaptic clefts. NE induces alpha-adrenergic stimulation and vasoconstriction which is the underlying culprit in organ damage [2]. We herein present a case of cocaine-induced splenic rupture with a review of the literature.
CASE REPORT

Splenic artery angiogram after placement of embolization coil showing patency of flow, no active extravasation.
The ‘Islands’ of preserved spleen lit up with IV contrast surrounded by a large collection of old blood and devitalized tissue.

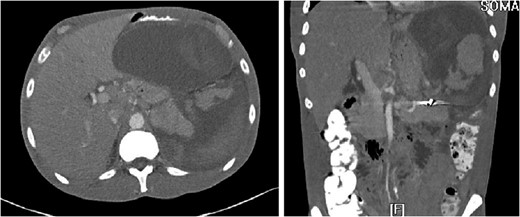
3D reconstruction and coronal CT after placement of pigtail drainage catheter.
DISCUSSION
Splenic rupture is a rare but serious complication from cocaine abuse. Given the ubiquitous prevalence of abuse and the potential for death from intraperitoneal bleeding, the prompt diagnosis and treatment of cocaine-induced disease including splenic rupture is essential.
Cocaine attains high concentrations within the spleen and the associated vasoconstriction has been shown to transiently reduce splenic volume on average by 20% [2]. Splenic hemorrhage may occur from arteriolar rupture from accelerated hypertension or from infarction and subsequent hemorrhage following resolution of vasospasm [1, 3]. The current management for the majority of splenic injury is a non-operative approach with adjunctive transcatheter splenic artery embolization (TSAE) which is effective for non-operative management in 90% of blunt splenic trauma [4]
Two general methods for TSAE of splenic injuries have been advocated. One option is coil embolization of the proximal splenic artery, which decreases arterial pressure in the spleen but allows continued perfusion through collateral arteries. The other method is superselective embolization of the bleeding arterial branch. To arrest the hemorrhage from splenic injury and to minimize infarct due to embolization, it is important to select appropriate method of TSAE on the basis of the features of arterial injuries [4–6]. Our patient was managed with coil embolization of the proximal splenic artery and subsequently maintained partial perfusion of splenic tissue.
A study conducted over an 11-year period reports that minor complications of fever, left-sided pleural effusions, and coil migration occur in 34% of patients while major complications of splenic abscess, infarction, cyst, and contrast induced renal insufficiency occur in 14% of patients who undergo TSAE. Of the patients in the study, ¾ of patients with major complications had undergone distal embolization, defined as distal to the main splenic artery trunk [7]. During the post-procedure course, our patient was noted to have minor complications of fever and left-sided pleural effusion as well as a major complication of intra-abdominal abscess.
It is generally recommended that patients who undergo emergent splenectomy receive pneumococcal, meningococcal and H. Influenzae (Hib) vaccinations 2 weeks postoperatively, however, the guidelines are unclear regarding post- TSAE patients [8]. 99.2% of active trauma surgeons immunize their postsplenectomy patients, whereas only 15.4% of surgeons immunize those who undergo splenorrhaphy and 8.4% immunize patients who are managed nonoperatively [9]. It has been proposed that the decision to vaccinate be based on splenic function post-TSAE. Based on CT volumetric analysis, coil embolization of the main splenic artery resulted in only a mild degree of splenic volume loss over the long term, with a mean of 15% decrease in volume. Patients that underwent distal TSAE demonstrated a 21% volume reduction while patients with proximal TSAE demonstrated a 4% reduction [10].
Our patient was vaccinated given that post-procedure CT showed the spleen to be partially necrotic with only two islands of well-perfused, preserved spleen depicting >15% decrease in splenic volume. The plan was to perform interval splenectomy however he was lost to follow up.
CONFLICT OF INTEREST STATEMENT
None declared.



