-
PDF
- Split View
-
Views
-
Cite
Cite
Yuni F Ongso, Han N Beh, Gastric band tubing-related complication during pregnancy, Journal of Surgical Case Reports, Volume 2017, Issue 11, November 2017, rjx241, https://doi.org/10.1093/jscr/rjx241
Close - Share Icon Share
Abstract
In the past few decades, laparoscopic adjustable gastric banding is one of the most common bariatric procedures performed to treat morbid obesity. Device-related complication such as connection-tubing problem is rare. Here we present a case of gastric band tubing complication during pregnancy. This case illustrates the need to maintain high index of suspicion of gastric band device-related complication during pregnancy and early referral for bariatric surgical assessment is recommended.
INTRODUCTION
Laparoscopic adjustable gastric banding is one of the most common bariatric procedure performed to treat morbid obesity in the past few decades. Its adjustability and reversibility make this procedure preferable to some patients and surgeons compared with other bariatric surgeries. Device-related complication such as connection-tubing problem is rare (~1%) [1]. Tubing-related complication in pregnancy is even rarer and it can be difficult to diagnose, as there are usually limited imaging modalities that can be used safely. Here we present a case of gastric band tubing complication during pregnancy.
CASE REPORT
A 27-year-old woman at 6 weeks gestation was admitted with 3 days of severe colicky periumbilical abdominal pain. This was associated with nausea. There was no vomiting, no reflux or dysphagia and the patient had reported normal bowel habit. Her observation parameters were within normal limits. Abdominal examination revealed tender periumbilical area without peritonism. This patient has had laparoscopic gastric band insertion 4 years prior. Her pre-procedure weight was 103 kg with body mass index (BMI) of 35.6 kg/m2. The band has been deflated completely 2 weeks prior to presentation as part of her antenatal care. She has no other comorbidities and no other prior surgical history. Her weight on admission was 75 kg with BMI of 25.9 kg/m2. Laboratories workup includes leukocyte count of 8.3 × 109/l and C-reactive protein of 22 mg/l. Ultrasound of the abdomen was unremarkable with normal intra-abdominal organs and viable single intrauterine pregnancy.
Given her ongoing symptoms, she underwent diagnostic laparoscopy. Prior to the procedure, the patient has requested for the gastric band to be removed instead of revised if the issue had been related to the device given that she had achieved satisfactory result (excess weight loss of 91%). Intraoperatively, it was found that the middle part of the tubing was wrapped around a loop of small bowel, creating an adhesion band around the bowel. The tubing and the gastric band were removed in a routine fashion with adhesionlysis of the adhesion band. The loop of bowel appeared compressed but viable and therefore left alone. The patient recovered well from the procedure and she was discharged home on Day 1 post procedure following a normal ultrasound confirming viable pregnancy. The patient was subsequently reviewed in clinic 4 weeks after the operation and she reported no further symptoms. Furthermore, her pregnancy was uneventful and she delivered a healthy baby at term (Figs 1 and 2).
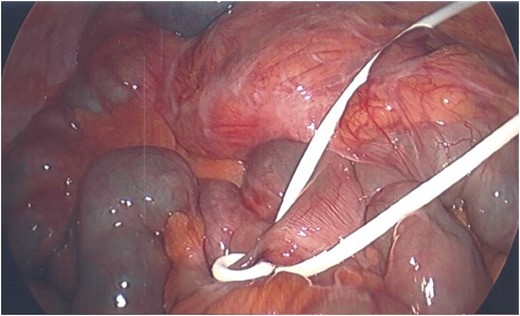

Scarring around small bowel mesentery with viable bowel loop after removal of device.
DISCUSSION
Gastric band tubing-related complications are rare with only limited published reports [2–5]. To our knowledge, this is the first reported tubing-related complication in a pregnant woman. Most reported cases during pregnancy involved slippage of band rather than tubing-related complication [6, 7]. Gastric band complications during pregnancy need to be acted on promptly as delay in management can be dangerous not only for the mother but fetus alike [8–10].
Tubing-related complication typically presents with symptoms of small bowel obstruction as a result of strangulation, internal hernia or bowel volvulus [2–5]. Our case posed a challenge in diagnosis. First, the patient presented with nonspecific abdominal pain with normal investigations. This was likely due to early presentation and, therefore, there were no symptoms of bowel obstruction. Second, her status of being pregnant posed a further challenge in the diagnosis as there were limited helpful imaging modalities that can be used safely without posing radiation risk. The decision to operate early was worthwhile. We believe that the delay in the operation could have led to patient developing bowel obstruction and subsequently strangulation. This case illustrates the need for practitioner to maintain high index of suspicion of gastric band device-related complication during pregnancy and early referral to bariatric surgeon is recommended.
CONFLICT OF INTEREST STATEMENT
None declared.
CONSENT
Consent has been obtained from patient for this case report.



