-
PDF
- Split View
-
Views
-
Cite
Cite
Ghada A Abu Jamea, Ammar C Al Rikabi, Khalid Akkour, Primary low-grade endometrial stromal sarcoma arising in the vagina: report of an unusual case and literature review, Journal of Surgical Case Reports, Volume 2017, Issue 11, November 2017, rjx238, https://doi.org/10.1093/jscr/rjx238
Close - Share Icon Share
Abstract
Endometrial stromal sarcoma rarely occurs as an extrauterine neoplasm and it is even more unlikely to be found in the vagina. To the best of our knowledge, only six cases of primary vaginal endometrial stromal sarcoma without association with endometriosis have been published to this day. We describe a case of a 58-year-old female with a history of vaginal heaviness caused by a mass lesion. After a biopsy was taken, the histopathological findings and immunohistochemical stains were consistent with low-grade endometrial stromal sarcoma. The patient underwent total hysterectomy and bilateral salpingo-oophorectomy with lymph node dissection followed by hormonal therapy. This line of management was heavily based on the treatment guidelines for endometrial stromal sarcoma.
INTRODUCTION
Endometrial stromal sarcoma (ESS) is a rare malignant neoplasm that is known to originate from the endometrial stromal cells. ESS accounts for only 0.2% of all uterine malignancies, for this reason it may sometimes be misdiagnosed as other more common types of malignancies [1]. The world health organization has recently reclassified ESS to low-grade ESS (LG-ESS), high-grade ESS (HG-ESS) and undifferentiated uterine sarcoma. This classification was based on the overall morphological resemblance of the lesion to proliferative-phase endometrial stromal cells, mitotic rate and clinical behavior [2]. Although LG-ESS seems to be relatively a more common subclass, it is still very unlikely to be found in extrauterine sites such as the vagina. We are reporting the case of a 58-year-old woman who was diagnosed to have primary vaginal LG-ESS without definitive association with endometriosis. The possible etiologies as well as literature review of similar cases are presented and discussed.
CASE REPORT
A 58-year-old woman (gravida 13, para 10) who became menopausal 10 years ago was referred to our hospital because of increasing heaviness in the vagina. Her past medical history was unremarkable except for hypothyroidism, hypertension and hypercholesterolemia which were all controlled by medication. Gynecological examination revealed a firm mass measuring 3 cm in max diameter and protruding from the left side of the vagina. She also had a small endocervical polyp measuring about 1 cm in max diameter. The ultrasound examination did not reveal any other abnormalities and an excisional biopsy from the cervical polyp showed a benign and inflamed endocervical polyp. A resection of the vaginal mass suggested a low-grade spindle cell neoplasm. However, a subsequent panel of immunohistochemical stains showed that the diagnosis is a LG-ESS most probably originating from vaginal stromal progenitor cells. The patient subsequently underwent a successful total abdominal hysterectomy with bilateral salpingo-oophorectomy and lymph node dissection (TAH-BSO-LND). There was no evidence of any primary endometrial neoplasm, metastatic disease or endometriosis in the resection specimen. The patient was prescribed Letrozole/Aromatase inhibitor 2.5 mg daily and discharged home. She remained well and disease free after 7 months of follow-up.
Pathological findings
The resected vaginal tumor consisted of an irregular and round firm mass measuring 3 cm in max diameter. The cut surface was white, solid and smooth. Histopathological sections showed that the lesion consisted of densely packed cells showing uniform spindle and oval nuclei. The mitotic rate was low (<5 per 10 high-power field), nuclear pleomorphism mild and there was no evidence of necrosis. The overall lesion appeared lobulated and intercepted by areas of hyalinization and increased vascularity. A diagnosis of low-grade spindle cell neoplasm was rendered pending the immunohistochemical stains (Fig. 1A and B). A large panel of immunohistochemical stains was done and it showed that the tumor cells are strongly positive for vimentin, CD10, estrogen (Fig. 2A and B) and progesterone with focal areas of positive staining for CD99. The proliferation marker Ki67 (MIB1) was positive in 10% of the tumor cells. The lesional cells were negative for h-Caldesmon, calponin, desmin, smooth muscle actin, CD68, CD34, Bcl-2, NSE, S100 protein, cyclin-D1, GFAP, HMB45, inhibin, EMA and synaptophysin. The morphological and immunohistochemical features in addition to the absence of endometrial stromal lesion elsewhere were entirely in keeping with primary LG-ESS.
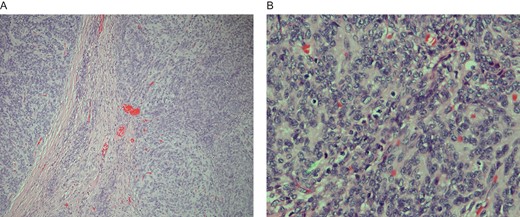
(A) Low-grade vaginal stromal sarcoma: section shows two separate but adjacent tumor nodules with a fibrous septum containing scattered tumor cells. Hematoxylin and eosin stain ×100. (B) High-power microscopic view of low-grade vaginal stromal sarcoma showing spindle and oval-shaped tumor nodules with mild nuclear pleomorphism and many scattered lymphocytes. The arrow head points to a mitotic figure. Hematoxylin and eosin stain × 400.
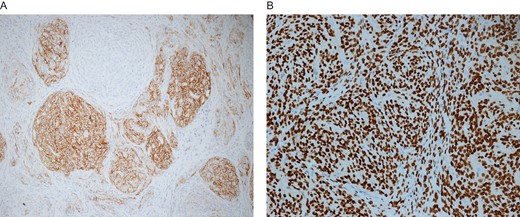
(A) CD10 positive immunohistochemical stain in tumor cells of low-grade vaginal stromal sarcoma. Immunohistochemical stain for CD10 × 100. (B) Strong positive nuclear staining of tumor cells for estrogen receptor marker. Similar pattern of positive nuclear staining was also seen with progesterone receptors. Immunohistochmeical stains for estrogen × 200.
DISCUSSION
LG-ESS is a rare malignant neoplasm that resembles the proliferative phase of endometrial stromal cells. The morphological appearance of LG-ESS displays a group of small, round to spindle shaped cells, with minimal atypia and variable mitotic activity. Positive immunohistochemical stains for CD10, estrogen receptor (ER) and progesterone receptor are evident features of LG-ESS. These results have correlated with our results, yet smooth muscle markers such as smooth muscle actin and desmin, which may be seen on some ESS, were not observed.
It is still unclear how primary extrauterine LG-ESS arises, in a study by Masnad et al. [3], and done on 63 patients with different extrauterine ESS, it was found that 60% of the patients had an association with endometriosis. This occurrence may explain the presence of ESS in extrauterine tissue, however our case and six other reported cases of primary vaginal LG-ESS had no detectable association with endometriosis. Alternatively, it is hypothesized, as suggested by Launchlan [4], that müllerian type stromal differentiation arising from coelomic epithelium is possible in extrauterine sites such as the fallopian tubes, ovaries and the pelvic peritoneum. This hypothesis cannot be applied to extrauterine sites which are not known to be derived from the coelomic epithelium such as the vagina.
Genetic abnormalities seem to play a role and they tend to include the JAZF1 gene. In a study by Chiang et al. [5], an assessment of the frequency of genetic rearrangements of endometrial stromal tumors demonstrated that four extrauterine ESSs had gene combinations of rearrangements in JAZF1-SUZ12andJAZF1-PHF1 and EPC1-PHF1 and PHF1-JAZF1, which were mutually exclusive in individual patients.
It has been established that LG-ESS is generally more common in younger women with a mean age between 45 and 57 [6]. However, affected older women had worse overall survival and progression [7]. Unlike the majority of patients with extrauterine ESS, our patient was not placed on any hormonal therapy before. She was also obese, thus a possibility of ER sensitivity to excess endogenous estrogen might have been associated in the development of the tumor [8].
Due to the rarity of the disease, there are no specific treatment guidelines to follow, and for this reason treatment is mainly based on previous case reports and treatment guidelines of ESS. Similar to the first non-endometriosis related primary vaginal ESS reported by Chang et al. [9], our patient underwent a hysterectomy with bilateral salpingo-oophorectomy and lymph node dissection. Our patient was also prescribed a dose of 2.5 of letrozol/aromatase inhibitor daily.
There is no doubt that the limited retrospective reported cases of primary vaginal LG-ESS is a challenging factor for determining the etiology of the disease as well as deciding the optimal treatment and prognostic factors in the patients affected. Further research done on a larger group of patients is, however, needed.
CONFLICT OF INTEREST STATEMENT
None declared.



