-
PDF
- Split View
-
Views
-
Cite
Cite
Eric J Weiner, Jordan J Ditchek, Rachele J Solomon, Stephanie Eyerly-Webb, Chauniqua Kiffin, Eddy H Carrillo, Dafney L Davare, A unique case of popliteal artery transection after a motorcycle collision, Journal of Surgical Case Reports, Volume 2017, Issue 11, November 2017, rjx222, https://doi.org/10.1093/jscr/rjx222
Close - Share Icon Share
Abstract
Popliteal artery injuries may have devastating consequences if not recognized in a timely fashion. The risk of delayed diagnosis of a vascular injury is particularly high in blunt trauma to the lower extremity. We present a case of popliteal artery injury that is unusual in two respects: severity (a complete transection in the setting of a blunt injury) and lack of clinical and radiographic signs of the commonly associated musculoskeletal injuries.
INTRODUCTION
Popliteal artery injury is relatively rare, and a delay in diagnosis and treatment can significantly increase morbidity [1–3]. The ligamentous fixation and anatomical proximity to the femur, tibial plateau and joint capsule render the popliteal artery susceptible to high-energy blunt and penetrating trauma [4]. The association between popliteal artery injury and tibiofemoral dislocations with or without spontaneous reduction, as well as femur fractures has been well described [2, 4–6]. In these cases, physical exams characteristically show severe cruciate ligament instability, and imaging studies demonstrate fractures, subluxations and/or soft tissue swelling [2, 5, 6].
Previous case series on popliteal artery injury following trauma have described intimal tears or ruptures of the popliteal artery upon exploration, but no complete transections [7]. We present a unique case of a complete left popliteal artery transection following a motorcycle collision (MCC), without any associated fracture or evidence of a tibiofemoral dislocation.
CASE REPORT
A 29-year-old male presented to the trauma center following a MCC. The Glasgow Coma Score was 5 at the scene, requiring immediate intubation. The systolic blood pressure was 98/50 mmHg, and the heart rate was 120 beats per minute. On physical examination, breath sounds were decreased to auscultation on the left, and a left chest wall deformity was noted. The left lower extremity was swollen and tense, and distal left lower extremity pulses were absent. A chest tube was inserted into the left hemithorax. Intravenous fluids and blood were administered, achieving only a transient improvement in vital signs. A focused assessment with sonography for trauma was negative. Radiographs of the left femur and left knee (Fig. 1a–c) demonstrated no evidence of fracture or dislocation. Due to continued hemodynamic instability and clinical evidence of left lower extremity compartment syndrome, the patient was taken emergently to the operating room.
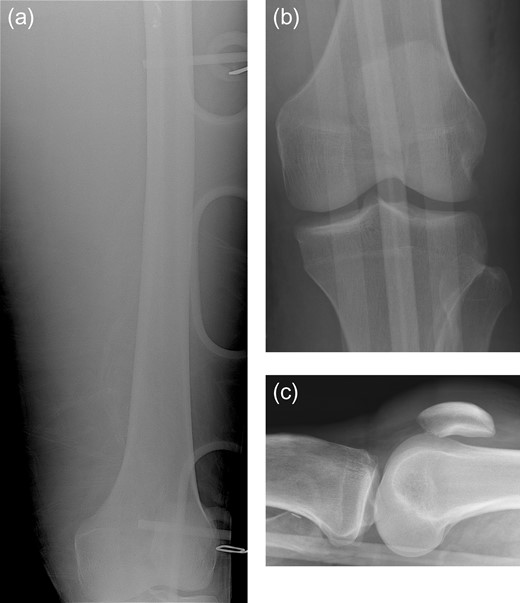
Portable frontal view of the left femur (a) obtained in the trauma bay demonstrates no evidence of acute fracture. Subsequent AP (b) and cross-table lateral (c) radiographs of the left knee demonstrate no evidence of acute fracture or dislocation.
The patient underwent fasciotomy of the left thigh with no return of his pulses. Following this, an intraoperative arteriogram was performed (Fig. 2), demonstrating extensive extraluminal extravasation of contrast from the popliteal artery and no opacification of arteries distal to the knee; these findings are consistent with popliteal artery transection. The patient had a left lower leg fasciotomy and vascular bypass, from the superficial femoral artery to the distal popliteal artery, using a contralateral saphenous vein graft, with successful restoration of distal pulses.
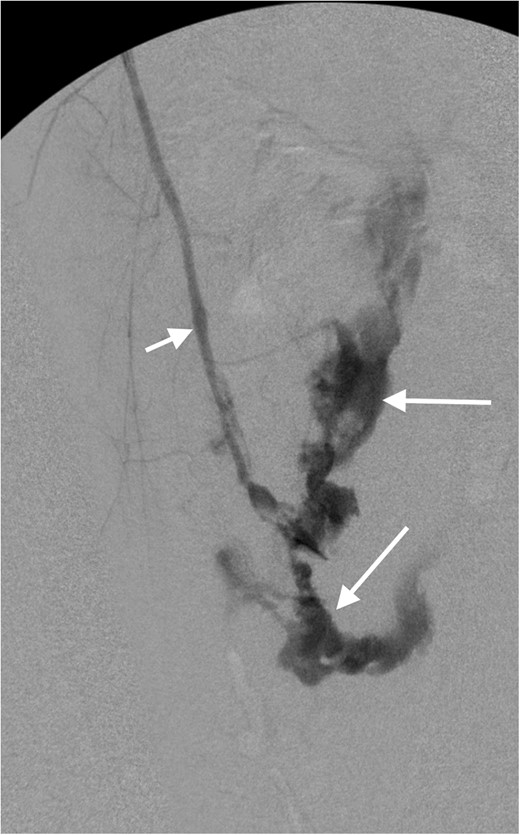
Intraoperative arteriogram of the left lower extremity demonstrates opacification of the superficial femoral artery (short arrow). There is extensive extraluminal extravasation of contrast (long arrows) from the popliteal artery, and non-visualization of the distal vessels, consistent with complete transection of the popliteal artery.
In addition to this injury, the patient suffered a traumatic brain injury, bilateral hemopneumothoraces and a spinal cord injury. Once stable, the patient was transferred to inpatient rehabilitation on hospital day 20.
DISCUSSION
Tibiofemoral knee dislocation is a rare and serious injury that occurs in ~0.02–0.1% of all musculoskeletal injuries [8]. These knee dislocations occur in both high- and low-energy blunt and penetrating traumas and often spontaneously reduce in the field [8]. Physical examination of the knee for ligamentous instability can alert the physician to the possibility of an occult knee dislocation [9]. It is imperative to recognize the clinical signs and symptoms of these dislocations, as they are associated with a significant incidence (20–40%) of concomitant popliteal artery injury, with ~1.6–13% of cases requiring acute popliteal artery repair [2, 8, 9]. Delayed diagnosis and treatment of a popliteal artery injury increases patient morbidity.
Popliteal artery injuries have been traditionally treated with open surgical repair and fasciotomy, although recent advances have allowed for endovascular repair in select patients. Endovascular techniques are generally implemented in hemodynamically stable patients to treat vascular injuries such as thrombosis, pseudoaneurysm, dissection, hematoma and arteriovenous fistula, and have been demonstrated to be successful specifically in instances of popliteal artery trauma [10–12]. A study using data from the National Trauma Data Bank to compare outcomes of open versus endovascular repair showed similar short-term clinical outcomes and hospitalization length between the two groups, and a lower rate of fasciotomy in the endovascular group [13].
In severe lower extremity trauma, clinical or radiographic evidence of distal femoral fracture or tibiofemoral dislocation should prompt careful vascular evaluation, which will often reveal the concomitant popliteal artery injury. In milder injuries, physical examination may demonstrate evidence of ligamentous instability, and radiographs may reveal only subtle findings such as non-displaced fracture, subluxation, joint effusion/lipohemarthrosis and soft tissue swelling. In these cases, a high clinical suspicion for popliteal artery injury must still be maintained. In fact, even in the absence of clinical or radiographic evidence of significant injury, vigilant evaluation for vascular injury is still warranted, as tibiofemoral dislocation often spontaneously reduces in the field, leaving little or no detectable deformity at the time the patient is clinically evaluated. Finally, in cases where no clinical history is available and the mechanism of injury is unknown, a severe vascular injury such as arterial transection should be considered as a potential cause of refractory hypotension.
CONFLICT OF INTEREST STATEMENT
None declared.



