-
PDF
- Split View
-
Views
-
Cite
Cite
Min P Kim, Edward Y Chan, Knotless suture allows for successful thoracoscopic diaphragm plication, Journal of Surgical Case Reports, Volume 2017, Issue 11, November 2017, rjx225, https://doi.org/10.1093/jscr/rjx225
Close - Share Icon Share
Abstract
Diaphragm paralysis can cause significant shortness of breath. This condition can be treated with diaphragm plication. We illustrate two cases where we used a knotless suture and total portal thoracoscopic technique to successfully plicate the diaphragm. A 70-year-old female with right-sided and a 44-year-old male with left-sided diaphragm paralysis. Both patients had a sniff test that showed paradoxical movement of the diaphragm. The port placements during the procedure were different due to the laterality but both patients had three 5-mm ports and one 12-mm port for the procedure. Plication was performed using the Endo Stitch knotless suture. Both patients went home on post-operative Day 1 without any complications. After 1 month, both patients had significant improvement in shortness of breath with resolution of the diaphragm elevation.
INTRODUCTION
Diaphragmatic paralysis is an abnormal elevation of the diaphragm due to a lack of innervation of the diaphragm that leads to paradoxical motion of the diaphragm. Traditional surgical treatment for symptomatic diaphragmatic paralysis has been thoracotomy [1] to plicate the diaphragm, flattening the diaphragm to eliminate the paradoxical motion and to help the other diaphragm function better. The surgical technique has evolved with video-assisted thoracoscopic surgical (VATS) diaphragm plication which still typically uses utility incision that is typically 3–6 cm [2] or a uniportal incision [3]. Although, it is an improvement to thoracotomy, the surgery still leads to significant pain. We illustrate how a knotless suture allows us to successfully complete a completely portal VATS approach to diaphragm plication.
CASE REPORT
The first case is a 70-year-old female with progressive shortness of breath. The patient had a CXR that showed an elevated right diaphragm (Fig. 1A) and sniff test showed a paralyzed right diaphragm. She underwent diaphragm plication (Video 1). On post-operative Day 1 (Fig. 1B) and 1 month follow-up (Fig. 1C), there was no longer an elevated right diaphragm.
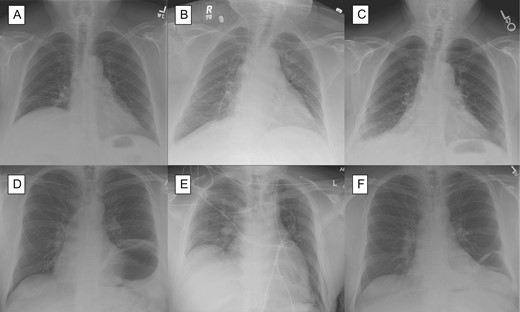
Chest X-ray for patient with right diaphragm paralysis (A) after repair on post-operative Day 1 (B) and after 1 month (C) as well as chest x-ray of patient with left diaphragm paralysis (D) after repair on post-operative Day 1 (E) and after 1 month.
The second case is a 44-year-old male with progressive shortness of breath over a year. The patient stated that his dyspnea had worsened over the past year. The patient had a CXR that showed an elevated left diaphragm (Fig. 1D) and sniff test showed left diaphragm paralysis. The patient had diaphragm plication. On post-operative Day 1 (Fig. 1E) and 1 month follow-up (Fig. 1F), there was no longer an elevated left diaphragm.
Surgical technique
Right side port placement
We placed a 5 mm Endopath XCEL® port (Ethicon, Somerville, NJ) in the fifth intercostal space along the tip of the scapula. Under direct vision, we passed the intercostal muscle and stopped prior to the diaphragm. The chest was insufflated to 10 mm Hg to allow us to see the angle between the chest wall and the diaphragm. We then placed a 12 mm trocar at the mid-axillary line in the sixth intercostal space and an additional 5 mm ports at the seventh intercostal space along the posterior axillary line to be used as an instrument port. We then placed a 5 mm trocar along the tip of the scapula in the ninth intercostal space as a camera port.
Left side port placement
We placed a 5 mm Endopath XCEL® port (Ethicon, Somerville, NJ) in the left upper quadrant of the abdomen and insufflated to 10 mm Hg to prevent any injury to the colon when plicating the diaphragm. We then placed a 5 mm Endopath XCEL® port (Ethicon, Somerville, NJ) in the fifth intercostal space in the mid-axillary line. This can be seen from the abdominal side to ensure safe port placement. We then insufflated the chest to 10 mm Hg and placed a 5 mm port along the tip of the scapula in the ninth intercostal space as a camera port. We then placed a 12 mm port in the seventh intercostal space in the mid-axillary line.
Plication
We placed a 0 V-LOCTM (Medtronic, Minneapolis, MN) permanent suture in the Endo StitchTM (Medtronic, Minneapolis, MN) through the 12 mm port. The diaphragm is plicated from the dome toward the chest wall from the right side to the left side layer by layer. Typically five layers of plication were performed to flatten the diaphragm (Video 1). Next, a 28 Fr chest tube was placed. The chest tube was removed the next day and the patients were discharged home the following day.
DISCUSSION
Patients with symptomatic diaphragm paralysis suffer from dyspnea. Diaphragm plication provides significant relief, but patients need to recover from the surgery. Traditionally, this has been performed with a thoracotomy, which in itself causes a significant amount of post-operative pain and recovery time. Some thoracoscopic approaches have significantly improved this outcome but still require a utility incision to assist in suture tying. Our study shows that this operation can be performed without the utility incision, which can provide significantly less pain with fewer incisions. There are VATS techniques where utility incision can be avoided by using intracorporeal knot tying but in our experience this is much more cumbersome and time consuming compared to use of knotless suture. Overall, use of knotless suture is a safe and effective way to perform diaphragm plication.
SUPPLEMENTARY MATERIAL
Supplementary material are available at the Journal of Surgical Case Reports online.
ACKNOWLEDGEMENTS
We thank Amma Saikin for language editing the manuscript.
CONFLICT OF INTEREST STATEMENT
M.P.K. and E.Y.C. have consulted for Medtronics, Olympus and Boston Scientific.
FUNDING
No funds were received for the current work



