-
PDF
- Split View
-
Views
-
Cite
Cite
Halil Olgun Peker, Nural Cafer Celik, Ulas Cikla, Mustafa K Baskaya, Metastatic prostate adenocarcinoma to intradural foramen magnum, Journal of Surgical Case Reports, Volume 2017, Issue 11, November 2017, rjx185, https://doi.org/10.1093/jscr/rjx185
Close - Share Icon Share
Abstract
Intradural metastatic tumors are rarely reported in foramen magnum (FM), including cases of melanoma, pituitary carcinoma, thyroid carcinoma, and prostate carcinoma metastases. We report a 68-year-old male who presented with right-sided headache, progressive swallowing difficulty requiring gastrostomy tube and hoarseness over the course of 1 year. Images revealed a heterogeneous, contrast-enhancing lesion in the FM that compressed the anterior aspect of the medulla and upper spinal cord. Although metastatic tumor was considered in differential diagnosis, presumptive diagnosis was FM meningioma due to lack of bone destruction or sclerosis on CT and T2W isointense and T1W hypointense appearance on MRI. The patient underwent gross total resection via right far-lateral transcondylar approach. Histopathological examination revealed prostate carcinoma metastasis. To the best of our knowledge this is the second case report of an intradural prostate carcinoma metastasis in the FM.
INTRODUCTION
Foramen magnum (FM) metastases are very rare, but a few case reports of intradural carcinoma metastases in that area have been published [1–4]. Metastatic prostate carcinomas (MPC) in the FM are exceedingly rare; as only one case study has been published in the literature [1]. The most common intracranial location for MPC are bone and epidural space.
CASE REPORT
A 68-year-old male presented with 10-pound weight loss over the course of the last month as a result of progressive difficulty with swallowing. The neurological examination revealed a diminished gag and a weak cough reflex. His tongue was deviated to the right with significant atrophy. MRI of the head revealed a heterogeneous, contrast-enhancing mass that was hypointense on T1 and isointense on T2-weighted images. It was 3.7 cm in diameter, located at right anterolateral part of the FM, compressing the medulla oblongata, extending into the hypoglossal canal and jugular foramen, and encasing the posterior inferior cerebellar artery (PICA) (Fig. 1).
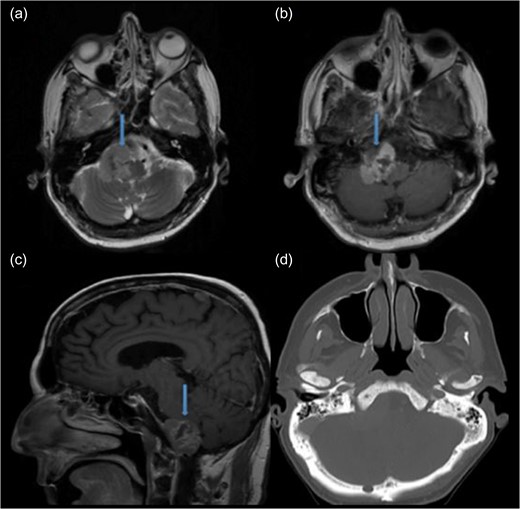
Preoperative MRI demonstrating an anterolateral right foramen magnum mass. (a) Axial T2-weighted MRI. (b) Axial T1-weighted contrast enhanced MRI. (c) Sagittal T1-weighted contrast enhanced MRI. (d) Axial CT image of brain shows no bone sclerosis or destruction.
The patient underwent microsurgical resection via far-lateral transcondylar approach in park bench position (Fig. 2a). The tumor was tan-colored and extremely firm, extending inferiorly to the entrance of the vertebral artery. It also extended into the hypoglossal canal and jugular foramen (Fig. 2b). The PICA, which was initially encased by tumor, and cranial nerve IX, X and XI were all preserved (Fig. 2c). Gross total resection was achieved (Fig. 2d). No changes of motor evoked potentials were observed throughout the surgery. The postoperative course was uneventful and images confirmed gross total resection (Fig. 3, video 1). Histopathological examination of the tumor revealed prostate adenocarcinoma metastasis positive for prostatic specific antigen. There was focal necrosis and a high proliferative index assessed by Ki 67.
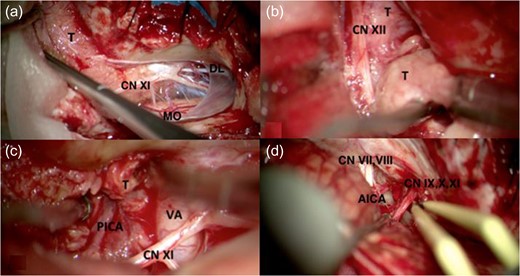
Intraoperative images showing (a) the T that was extrinsic to the cerebellum and medulla oblongata (MO), was pushing CN XI medially and encasing dentate ligament (DL). (b) CN XII encased by T. (c) PICA and Vertebral Artery (VA) encased by T. (d) After tumor resecting cranial nerve VII, VIII (CN VII, VIII), anterior inferior cerebellar artery (AICA) and CN IX, X, XI preserved.
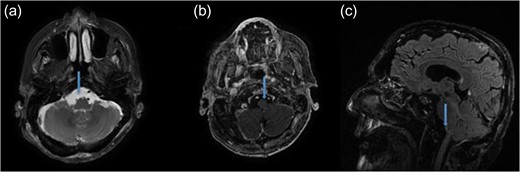
Postoperative MRI demonstrating the gross total mass resection. (a) Axial T2-weighted MRI. (b) Axial T1-weighted contrast enhanced MRI. (c) Sagittal T1-weighted contrast enhanced MRI.
DISCUSSION
Skull base metastases occur in 4% of all cancer patients [5]. The most frequent primary lesions that metastasize to the skull base are breast, lung, and prostate cancers. Most of these are localized in the parasellar region, middle fossa and anterior fossa [5–7]. Prostate carcinoma represents 17–38% of reported skull base metastases according to recent retrospective reviews [5, 8]. Intradural metastases are rare in the FM, and a few case reports have been published in literature including melanoma, pituitary, thyroid carcinoma metastasis [2–4]. Only one intradural prostate carcinoma metastasis exists in the literature other than our case [1].
Gadolinium-enhanced brain MRI is the gold standard to diagnose FM metastases [6]. The FM metastases show hyperintensity on T2 and hypointensity on T1 with variable contrast-enhancement. CT is also important to show bone destruction or sclerosis especially for prostate adenocarcinoma [6]. Interestingly, FM metastases can mimic subdural hematoma and meningioma [1, 9]. With the current case no bone invasion was detected by CT scans. Radiologically our case was similar to meningioma regarding the following features: isointensity on T2, hypointensity on T1 in MRI and no bone destruction or sclerosis in CT images (Fig. 1).
Radiotherapy and stereotactic radiosurgery are used for the treatment of skull base metastases in some of cases. The main limitations of these treatments are giant tumor size and proximity to the brainstem. For chemo-sensitive or hormone-sensitive lesions, chemotherapy or hormonotherapy might be beneficial [7, 10].
Although surgery is indicated in only a few cases of metastatic tumors in FM, it is life-saving and beneficial for symptom resolution in patients who has rapid neurological deterioration. Furthermore, patients who have tumors without any pathological confirmation or relatively radiotherapy resistant tumors such as melanoma, renal cell carcinoma and sarcoma should be considered for surgery. The appropriate candidates for the surgery are patients who have controlled systemic disease, a long life expectancy and a high Karnofsky performance score [7, 10].
Metastatic prostate adenocarcinoma to the intradural FM is rare and difficult to manage. Although the first treatment option is radiotherapy and stereotactic radiosurgery, surgery can offer benefits regarding symptom resolution and control of disease progression. Establishing a multidisciplinary management approach is necessary for metastatic lesions in FM.
SUPPLEMENTARY DATA
Supplementary material is available at the Journal of Surgical Case Reports online.
CONFLICT OF INTEREST STATEMENT
All the authors declare no conflict of interest.
REFERENCES
- magnetic resonance imaging
- deglutition disorders
- headache
- heterogeneity
- hoarseness
- differential diagnosis
- foramen magnum
- melanoma
- meningioma
- neoplasm metastasis
- sclerosis
- diagnosis
- spinal cord
- prostate cancer
- thyroid carcinoma
- gastrostomy tubes
- histopathology tests
- pituitary carcinoma
- bone destruction



