-
PDF
- Split View
-
Views
-
Cite
Cite
Jennifer M. Nishimura, Ted Farzaneh, Alessio Pigazzi, Pneumatosis coli causing pneumoperitoneum, Journal of Surgical Case Reports, Volume 2017, Issue 1, January 2017, rjw233, https://doi.org/10.1093/jscr/rjw233
Close - Share Icon Share
Abstract
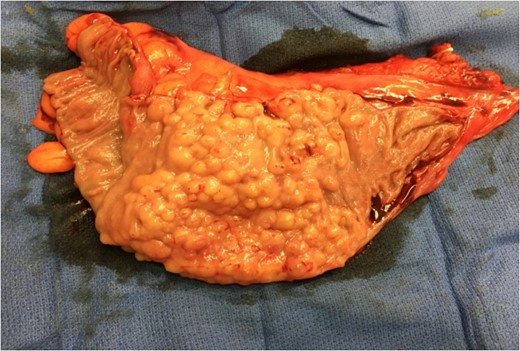
This is a case of a 54-year-old gentleman who presented to an outside hospital emergency department with lower abdominal pain. Computed tomography imaging showed a small amount of intraperitoneal free air and cystic pneumatosis coli. He was admitted, managed conservatively with intravenous antibiotics, and then discharged home after his symptoms improved. Elective laparoscopic sigmoid colectomy was subsequently performed with intraoperative findings of partial sigmoid volvulus and extensive pneumatosis coli of the sigmoid colon. Pneumoperitoneum was determined to be from ruptured intramural cysts. The etiology of pneumatosis coli was likely from chronic sigmoid volvulus.
INTRODUCTION
Pneumatosis cystoides intestinalis (PCI) is a rare finding characterized by multiple air-filled cysts in the submucosa, subserosa and/or muscularis propria of the intestine. Recent studies report that PCI or pneumatosis intestinalis is more frequently found in the colon than the small bowel [1, 2]. When located in the colon, it is specifically termed pneumatosis coli.
PCI is not well understood. Symptoms associated with it are non-specific, commonly including abdominal pain and distension, diarrhea, bloody stool and constipation [1]. The underlying pathology is diverse and not always identified. The presence of PCI can be an incidental finding of no clinical significance; however, it can also be a sign of an underlying disease process such as bowel necrosis, mesenteric ischemia and bowel obstruction which can be life-threatening. When a serious underlying intra-abdominal pathology is suspected, urgent surgical intervention is warranted.
We present a case of pneumatosis coli and pneumoperitoneum in an otherwise healthy male patient.
CASE REPORT
A 54-year-old gentleman with 30 pack year history of smoking, chronic constipation and symptoms of irritable bowel syndrome presented to an outside hospital emergency department (ED) with 5 days of lower abdominal pain and cramping. The pain was initially very mild in nature, but suddenly became severe a few days after onset. The pain then subsided, but did not completely resolve.
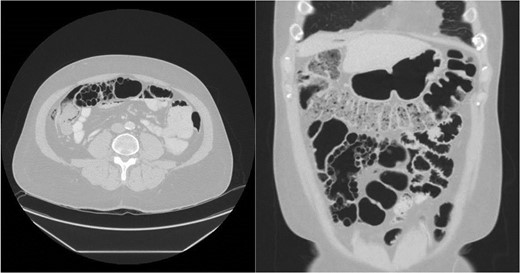
CT abdomen pelvis with IV contrast demonstrating cystic pneumatosis coli.

Multiple submucosal air pockets (cysts) ranging in size from 0.3 to 1.5 cm.
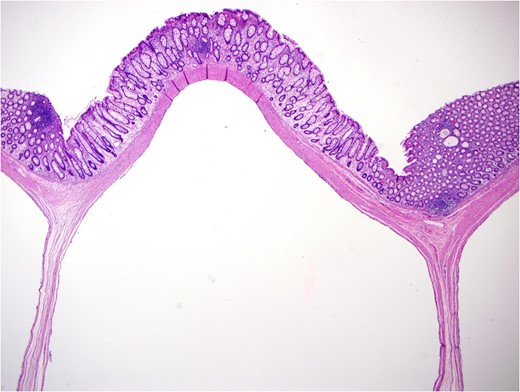
Microphotograph: multiple cystic spaces in submucosa and muscularis propria, with mild hyperplastic mucosal changes. H&E stain, original magnification ×40.
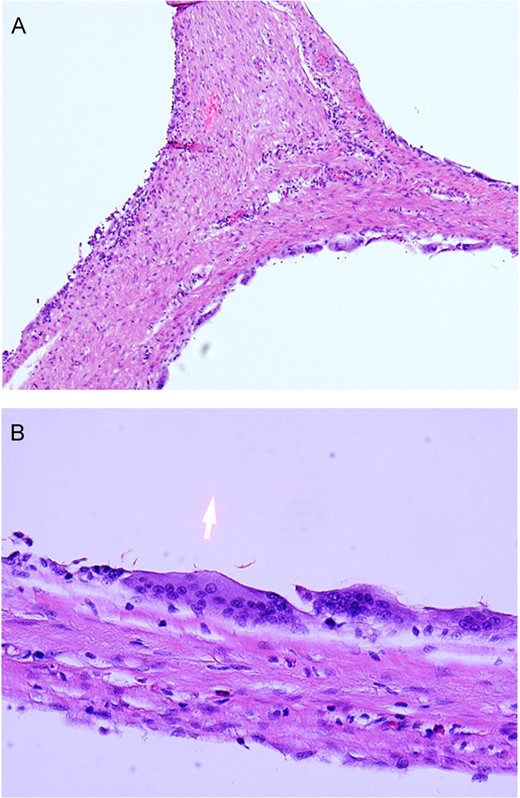
Microphotographs: cystic spaces are lined by histiocytes and multinucleated giant cells. H&E stain, original magnification ×200 (A) and ×400 (B).
DISCUSSION
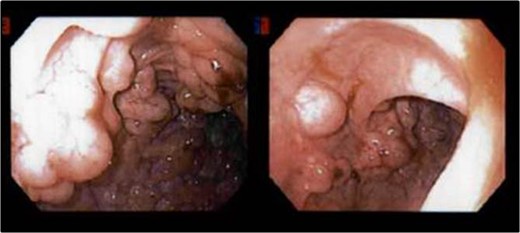
In this case report, we describe a patient who initially presented with symptomatic pneumatosis coli and pneumoperitoneum of undetermined etiology. Despite the imaging findings, his entire clinical picture did not warrant emergent surgical intervention, and he was managed conservatively as an inpatient. He was discharged home and additional work-up was performed on an outpatient and elective basis, revealing multiple sigmoid hyperplastic polyps without evidence of transmural colonic perforation.
Pneumoperitoneum in association with PCI can be secondary to viscus perforation or ruptured intramural cysts [3]. When this patient initially presented to the ED, he had free air on CT concerning for colonic perforation. However, further work-up determined the source of pneumoperitoneum was likely from ruptured intramural cysts as there was no evidence of gross transmural perforation intraoperatively and on final surgical pathology of the sigmoid colon. This correlates with his benign clinical picture.
The underlying pathology of PCI is diverse and not always identified. Sigmoid volvulus has been reported as both an etiology and a complication of PCI [4]. Here, we favor chronic sigmoid volvulus as the etiology rather than a complication of PCI. He had a redundant sigmoid colon, short mesenteric attachment and history of constipation, predisposing him to sigmoid volvulus. His presentation of recurrent abdominal pain with resolution may be due to recurrent torsion and spontaneous detorsion.
This case describes chronic sigmoid volvulus as a potential etiology of PCI and ruptured intramural cysts resulting in pneumoperitoneum.
REFERENCES
- computed tomography
- cysts
- emergency service, hospital
- intraoperative care
- laparoscopy
- pneumatosis cystoides intestinalis
- rupture
- sigmoid colon
- diagnostic imaging
- pneumoperitoneum
- sigmoid volvulus
- colectomy, sigmoid
- abdominal pain, lower
- intraperitoneal infusion
- antibiotic therapy, intravenous
- causality



