-
PDF
- Split View
-
Views
-
Cite
Cite
K. Laeeq, S. Cheung, B. Phillips, Hemoperitoneum secondary to intercostal arterial bleeding in a trauma patient, Journal of Surgical Case Reports, Volume 2017, Issue 1, January 2017, rjw194, https://doi.org/10.1093/jscr/rjw194
Close - Share Icon Share
Abstract
Blunt trauma resulting in rib fractures can be associated with hemothorax, pneumothorax, pulmonary contusions or less frequently chest and abdominal wall hematomas. Our case describes the first report of hemoperitoneum secondary to intercostal arterial bleeding from blunt trauma in a patient on anticoagulation.
INTRODUCTION
Blunt trauma resulting in multiple rib fractures can be associated with intercostal bleeding [1]. There are multiple reports of intercostal arterial bleeding resulting in abdominal wall hematomas [2] and hemothorax [1] that require embolization [3] or even thoracotomy [4]. To our knowledge however, this is the first description in the literature demonstrating hemoperitoneum from intercostal arterial bleeding requiring laparotomy.
CASE REPORT
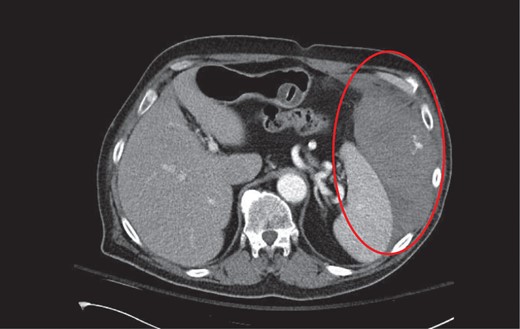
CT axial with intravenous contrast demonstrating a large left abdominal wall hematoma with active contrast extravasation from an intercostal artery.
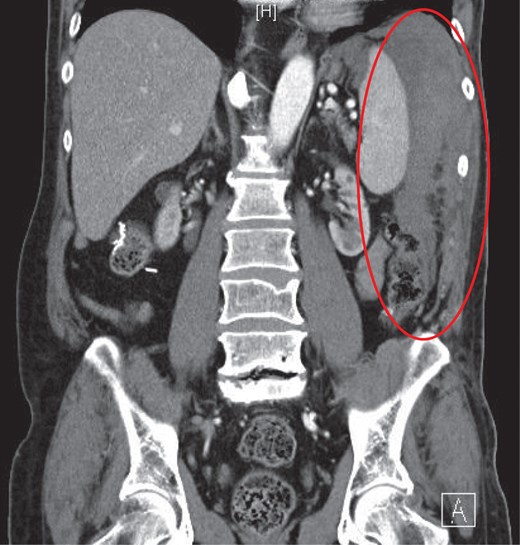
CT coronal with intravenous contrast demonstrating intraperitoneal blood products within the perisplenic region and left paracolic gutter.
DISCUSSION
Blunt thoracic trauma is often associated with rib fractures that may disrupt nearby structures including intercostal and internal mammary vasculature [1]. Such injuries can be associated with hemothorax, pneumothorax, pulmonary contusions and the development of an extrapleural hematoma that has a reported incidence of 7.1% [5].
In this report, the patient presented with hemoperitoneum from intercostal arterial bleeding. Clinically stable patients with normal hemodynamic parameters and radiographic features consistent with a non-expanding hematoma can be monitored in the intensive care unit with serial abdominal exams, laboratory studies, and reversal of coagulopathies [6]. In this situation, the patient was on dabigatran etexilate which is an oral prodrug converted by a serum esterase to dabigatran, a potent, direct, competitive inhibitor of thrombin [7]. Idarucizumab was used to reverse our patient's coagulopathy; it is an FDA-approved reversal agent for dabigatran and has shown to completely reverse the effects of dabigatran within minutes [8]. Idarucizumab is a monoclonal antibody fragment that binds dabigatran with an affinity that is 350 times greater than thrombin [8]. If unavailable, vitamin K, prothrombin complex concentrate, or fresh frozen plasma can be used in an attempt to reverse anticoagulation.
For patients presenting with rapidly expanding extrapleural hematomas, hemodynamic instability, or persistent bleeding from intercostal arterial branches, options for intervention include transcatheter arterial embolization (TAE) or surgical exploration [1, 4]. TAE has been reported as a safe and reliable technique in the management of blunt intercostal arterial injury associated with clinical deterioration [1]. In our patient, TAE was undertaken shortly after his arrival to our trauma center but did not reveal an active source of bleeding.
Surgical exploration should be considered with failure of angioembolization or when interventional radiology is not available. Strategies for operative exploration are dependent on the clinical scenario, hemodynamic stability, and the impact of associated injuries. In our case, a left-sided subcostal incision allowed access superiorly to the involved intercostal artery as well as inferiorly to evacuate the hematoma. Surgical plication of the suspected area was conducted and the tear in the periotneum was repaired during our fascial closure. At the end of the operation satisfactory hemostasis was achieved and we did not feel the need to place a drain.
In conclusion, hemoperitoneum secondary to intercostal arterial bleeding is an uncommon clinical finding. This can be managed with angioembolization if resources are available. Immediate reversal of medically-induced coagulopathy is also indicated. In patients with hemodynamic instability, expanding hematoma, or active contrast extravasation that cannot be embolized, surgical exploration should be entertained.
CONFLICT OF INTEREST STATEMENT
None declared.



