-
PDF
- Split View
-
Views
-
Cite
Cite
Ali Kordzadeh, Bruno Lorenzi, Jiten P. Kalyan, Muhammad A. Hanif, Alexandros Charalabopoulos, A rare presentation of an acute appendicitis, Journal of Surgical Case Reports, Volume 2017, Issue 1, January 2017, rjw232, https://doi.org/10.1093/jscr/rjw232
Close - Share Icon Share
Abstract
Paraumbilical hernia sac usually contains omentum, bowel loop and rarely appendicular epiploicae, metastatic deposits and vermiform appendix. Presentation of acute appendicitis in a paraumbilical hernia is rare and limited to few case reports in the literature. Herein, we would like to report a case of a successfully treated acute appendicitis presenting in a paraumbilical hernia in an 84-year-old lady with 6-month follow-up.
INTRODUCTION
Paraumbilical hernia occurs as a result of congenital incomplete closure of the fetal umbilical defect. Their reported incidence is estimated 10% in Caucasian and almost 90% in African population. They present as a lump and/or swelling commonly associated with abdominal discomfort and the majority are reducible; however, strangulation is not uncommon. The most common content of the sac is omentum, bowel loop and surgical repair remains the only definitive treatment [1, 2]. Appendicitis within the hernia sac has been reported in the inguinal (Amyand hernia) and femoral region (De Garengeot hernia); however, their presence in the paraumbilical hernia is extremely rare and a search of the literature demonstrated three previous perorated cases [3]. Herein, we would like to report a case of a successfully treated acute appendicitis presenting in a paraumbilical hernia in an 84-year-old lady with 6-month follow-up.
CASE REPORT
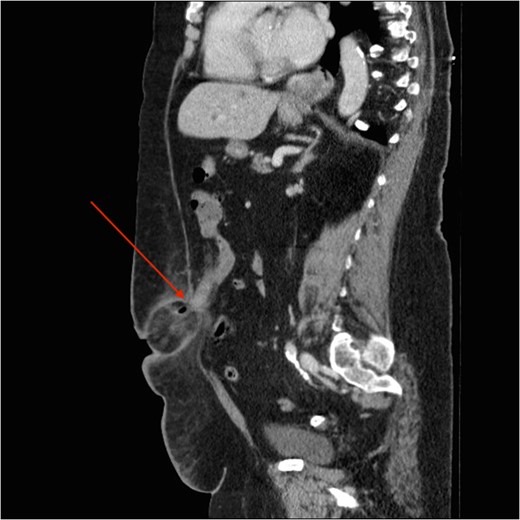
Sagittal slice of the CT demonstrating the paraumbilical sac containing cecum and appendix along with fat stranding and air loculation and narrow neck (red arrow).
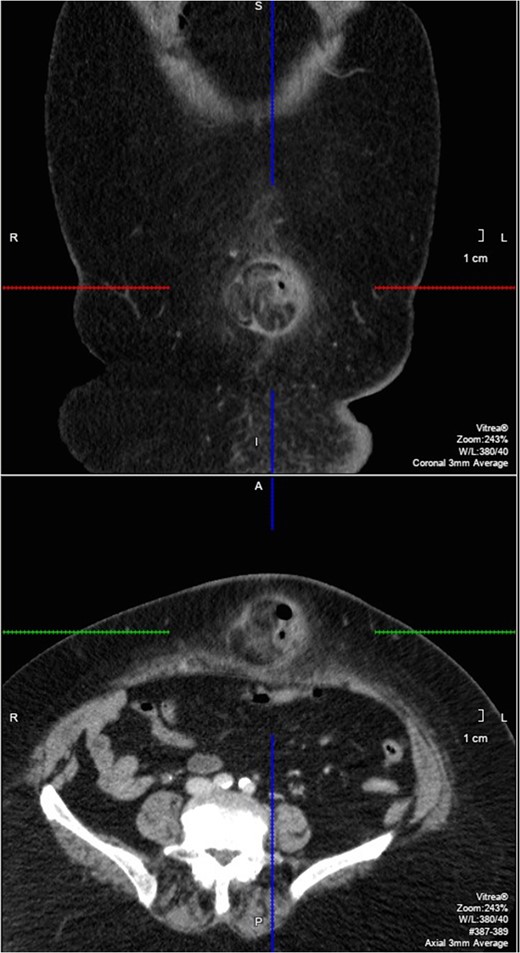
Coronal and axial slice of the CT showing the paraumbilical hernia (within marked areas).
The decision was made to operate and the patient was taken to the operating room for the repair of the paraumbilical hernia under general anesthesia. A midline incision (mini laparotomy) was made and the hernia sac was exposed. The sac contained viable cecum and inflamed necrotic appendix. Therefore, a mayo repair with full reduction of the viable cecum back into the abdominal cavity following sac excision and appendectomy was performed. Histopathological examination 3 weeks later confirmed the diagnosis of acute appendicitis. The patient made an uneventful recovery and was discharged 5 days later with no postoperative complication on 6-month follow-up.
DISCUSSION
Acute appendicitis remains the most common surgical emergency to date and their presentation can vary, however, the majority present with the classical symptoms of central to right iliac fossa abdominal pain, nausea, anorexia and vomiting. This is related to the anatomical position of the appendix from developmental phase of intestinal rotation. Ryan et al. review of n = 8692 cases of acute appendicitis, demonstrated that 0.13% of all appendicitis could present within the incisional, inguinal, femoral and obturator hernia [4]. The incidence of appendicitis in a paraumbilical hernia remains unknown and an extensive search of literature in the English language highlighted only three prior cases that presented with peroration and pus collection.
It remains unclear how the cecum and appendix can freely mobilize to the midline and present themselves within the sac of a paraumbilical hernia. It has been suggested that in 10% of the population, there might be an anatomical variation and abnormal cecum mobility otherwise referred to as mobile cecum syndrome [5]. In such individuals, the lateral peritoneal attachment of cecum is either absent or so mobile that terminal ileum and cecum can be found in any quadrant of the abdomen depending on the position and activity of the patient [6]. In addition, acute inflammatory response (appendicitis) and subsequent intraabdominal events (localization, adhesion and abscess) and the presence of a prior defect (paraumbilical) could explain such presentation. Another explanation in such circumstances is appendicitis as a result of extrinsic pressure, strangulation and necrosis within the hernia defect. However, it is difficult to establish which pathophysiological process (or perhaps both) could have attributed to this rare presentation.
Clinical examination remains vital in such cases (irreducible hernia) and arguably CT remains the best investigative modality of the choice in doubtful and complicated circumstances specially when there is a suspicion of malignancy due to old age [7]. However, the only definitive treatment is surgery for both appendicitis and strangulated hernia, and detailed examination of the sac contents remains crucial before their reduction into the abdominal cavity. Following an appendectomy, primary repair over mesh repair due to later incidences of mesh infection is highly recommended.



