-
PDF
- Split View
-
Views
-
Cite
Cite
Thomas J.G. Chase, Joshua Luck, Lauren S. Harris, Gareth Bashir, Conservative management of migrated percutaneous endoscopic colostomy tube, Journal of Surgical Case Reports, Volume 2017, Issue 1, January 2017, rjw227, https://doi.org/10.1093/jscr/rjw227
Close - Share Icon Share
Abstract
A 68-year-old male nursing home resident presented following dislodgement of a percutaneous endoscopic colostomy (PEC) tube originally sited to prevent recurrent sigmoid volvulus. Computed tomography demonstrated tube migration into the lumen of the recto-sigmoid junction, where it remained for 12 days before passing spontaneously. During this period, the patient remained asymptomatic; the residual colocutaneous fistula functioned as a decompressive valve. Originally, the patient was due to be discharged with early flexible sigmoidoscopy follow-up. However, complex social issues delayed discharge. During his admission, a second PEC tube was successfully inserted next to the previous colostomy site without complication. This is an unusual case and no similar episodes of asymptomatic PEC migration have been reported. We demonstrate that such cases may be offered an appropriate trial of conservative management. Here, we describe our experience and critically appraise the literature.
INTRODUCTION
Sigmoid volvulus is the third most common cause of colonic obstruction in adults and is associated with high morbidity and mortality [1, 2]. Despite this, there is significant disagreement regarding management [3] with a lack of randomized controlled trials to guide best practice [4]. Current consensus is—in the absence of ischaemic, gangrenous or perforated bowel requiring emergency surgery—to attempt decompression using flexible sigmoidoscopy or colonoscopy [1]. If successful, early elective surgery may be offered, typically involving a limited sigmoid resection with primary anastomosis [2, 3, 5]. If decompression is unsuccessful, emergency surgery is indicated [2, 5].
Sigmoid volvulus is more common in elderly patients [5, 6], the majority with comorbidities [4]. These can make patients unsuitable for surgical intervention, as in our case. Non-operative options include: endoscopic T-fastener fixation, tube sigmoidostomy, colon extraperitonealization, mesocoloplasty, sigmoid plication, Ladd's procedure or percutaneous endoscopic colostomy (PEC) tube placement [4]. Although no trials have directly compared these various options, PEC insertion is usually preferred due to its lower risk profile [7, 8]. The most common complication following PEC insertion is infection—occurring in up to 77% of patients—which may necessitate PEC removal [9].
Here, we present the first case of asymptomatic PEC tube migration and demonstrate how an appropriate trial of conservative management may be offered.
CASE REPORT
A 68-year-old nursing home resident presented to the Emergency Department after his family noticed his PEC tube was missing.
The PEC tube was inserted 8 months earlier following recurrent sigmoid volvulus requiring repeated flatus tube decompressions. It was intended to provide definitive, long-term management; comorbidities including multiple strokes and poorly controlled diabetes meant more invasive options were unsuitable.
The PEC tube had become dislodged after a healthcare worker accidentally removed a skin clip. This led to the surgical ward nursing staff—with the family's support—raising a ‘Safeguarding of Vulnerable Adults’ (SOVA) concern.
The patient remained asymptomatic with a soft, non-tender abdomen. The only abnormal clinical finding was the absence of a PEC tube from a patent periumbilical colostomy site.

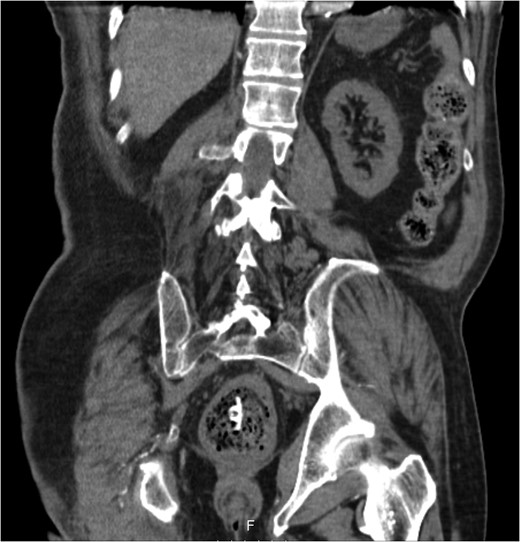

The patient remained well and the PEC tube passed spontaneously on Day 12, during a bowel motion.


The patient was discharged following clearance by social services. All staff at the nursing home attended educational sessions, run by the community stoma care nurse, to ensure safe future PEC management.
DISCUSSION
Our patient was unfit for major surgery and his recurrent sigmoid volvulus was managed conservatively with PEC fixation. Other comparable patients have been treated similarly elsewhere [7–10].
A number of clinical decisions had to be made during this admission:
If and how to remove the PEC tube?
Tube migration leading to perforation and frank peritonitis has been described elsewhere [10]. However, there are no cases of asymptomatic dislodged PEC tubes. Following discussion with gastroenterology and colorectal surgery, the decision was made to let the PEC pass spontaneously or remove it during early follow-up flexible sigmoidoscopy. The PEC tube was naturally expelled on Day 12 without complication.
Does the PEC tube need to be replaced?
The literature does not give a clear answer. Several case reports suggest that keeping the PEC tube in situ prevents volvulus recurrence [8, 10] and, if removed, symptomatic relapse is likely [7, 8, 10]. Infection [9] or patient request [10] often necessitates early PEC removal at a known risk of recurrence [9].
Should the bowel be fixed at one or two points (i.e. one or two PEC tubes)?
As with other examples [6], this patient's bowel was fixed originally with one PEC. However, effective, long-term prevention typically involves the insertion of two PEC tubes, ideally at each end of the sigmoid colon to reduce mesenteric mobility. This is usually well tolerated with good outcomes [7, 8, 10]. Indeed, in a case where one of two PEC tubes was removed, the patient experienced volvulus recurrence and a second tube had to be re-sited [10].
In our case, only one PEC tube was re-inserted. This was due to technical difficulties at sigmoidoscopy; however, we were reassured by the fact that our patient had not had volvulus recurrence with a single PEC previously. It was thought that the residual colocutaneous fistula tract, obliterated by granulation tissue, may affix the bowel to the anterior abdominal wall at a second location.
In the 9 months since PEC re-insertion, the patient has not had any further episodes of volvulus.
After how many episodes of sigmoid volvulus should prophylactic PEC placement be offered?
The literature is inconclusive. One study (of six patients) reported that the mean number of episodes before PEC placement was 3.5 [7], but no larger trials have been conducted. Typically, intervention is offered on a case-by-case basis with emphasis on patient preference in those unsuitable for operative intervention.
CONCLUSION
This is the first published report of PEC migration into the large bowel without obstruction or perforation. We demonstrate that an appropriate trial of conservative management may be offered whilst decisions are made as to long-term prophylaxis. To what extent the residual tract may help to affix the bowel to the abdominal wall remains unknown.
ACKNOWLEDGEMENTS
All authors contributed to the manuscript. T.J.G.C. drafted the original manuscript before being reviewed and edited by J.L., L.S.H. and G.B. We would also like to thank North Middlesex General Surgery department for contributing towards submission costs.



