-
PDF
- Split View
-
Views
-
Cite
Cite
Josep Torrent, Alberto Bailez, Jordi Asuncion, Recurrence of an intra-articular osteoid osteoma of the great toe: a case report and review of the literature, Journal of Surgical Case Reports, Volume 2017, Issue 1, January 2017, rjw226, https://doi.org/10.1093/jscr/rjw226
Close - Share Icon Share
Abstract
Osteoid osteoma (OO) is a benign tumor that it is not generally seen in the foot and even less frequently in the phalanx (2–4%). The diagnosis when its location is intra-articular is a challenge and often delayed because the symptoms mimic a real arthritis. We report a clinical case involving a 16-year-old male patient who complained of persistent pain of the interphalangeal joint (IPJ) of the left hallux. A juxta-articular OO of the condyle of the proximal phalanx was identified. The patient underwent surgery that included tumor removal preserving the articular cartilage. After a non-complete nidus resection, there was a recurrence. The patient underwent surgery with a removal en-block of the distal part of the proximal phalanx and fusion of the IPJ with interposition of a tricortical autograft. After a follow-up of 30 months, the X-ray showed total arthrodesis of the joint without signs of recurrence or pain.
INTRODUCTION
Osteoid osteoma (OO) accounts for 10% of all benign bone-forming tumor. It appears most often in the second and third decades of life, more commonly in men [1]. The most frequent location is in the cortical region of the diaphysis of long bones. It is not generally seen in the foot and even less frequently in the phalanx (2–4%) [2]. Bergstrand in 1930 was likely the first to describe two cases.
The typical clinical presentation is predominantly nocturnal severe pain [1].
However, it must be included in the differential diagnosis of rheumatoid diseases when the tumor is intra-articular, because the involvement of the articular cartilage can provoke articular effusion or joint stiffness which may mask the clinical diagnosis [3].
When the tumor affects the cancellous bone, the typical image of nidus is not produced making the diagnosis even more difficult [4].
REPORT
We are reporting a case of OO of the hallux proximal phalanx in a 16-year-old male. The patient complained of persistent pain and stiffness of the interphalangeal joint (IPJ) of the left hallux and difficulty in walking for a duration of 10 months. There was no preceding history of significant trauma.

Posterior–anterior X-ray imaging of the left forefoot, showing an intra-articular osteolytic lesion (arrow) in the condyle of the proximal phalanx of the hallux.
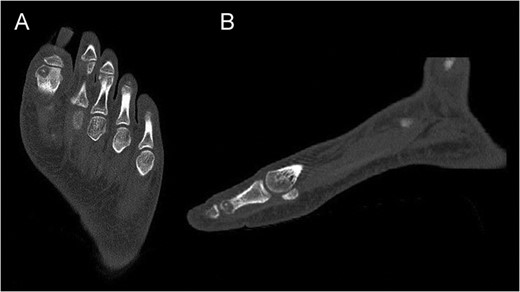
Preoperative CT of the proximal phalanx of the left hallux: axial (A), and sagittal view (B), showing the osteolytic nidus of the tumor with central calcification surrounded by a slight sclerotic halo: the standard image of OO.
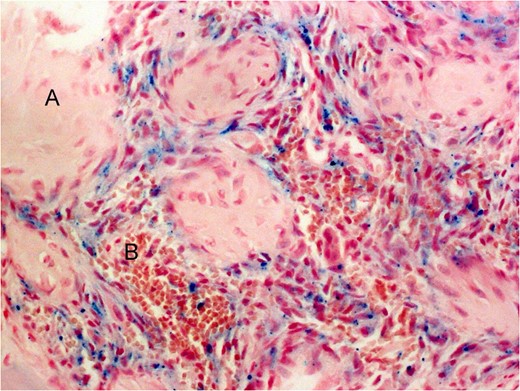
Histological image of the lesion. (A) Woven bone. (B) Blood vessels (original magnification ×40, Perls tintion).

Posterior–anterior (A) and oblique (B) X-ray imaging of the left forefoot, showing the integration of the bone graft after 6 weeks.
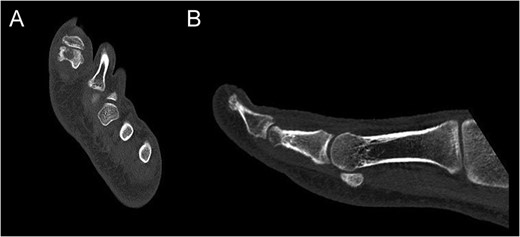
CT of the proximal phalanx of the left hallux: axial (A) and sagittal view (B), showing the recurrence of the OO and its extension to the articular surface.

Intraoperative image of the hallux showing the interposition of a tricortical autograft preserving the length of the big toe.
The pain decreased post operation with no rest-pain after 3 weeks. After 6 weeks, the X-ray revealed radiological signs of consolidation which allowed for weight bearing. Four months after surgery, the patient returned to sport without limitations.
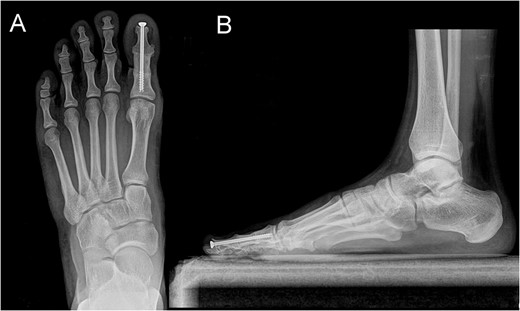
Posterior–anterior (A) and lateral (B) X-ray imaging of the left foot, showing the arthrodesis without signs of recurrence after a follow-up of 30 months.
DISCUSSION
The most common localization of OO are diaphyseal and metaphyseal regions of long tubular bones comprising approximately 50% of all reported cases [3].
The foot is very rarely involved. In a review of a series of 860 cases of OO, Jackson found an incidence of <4% in the foot [2, 5, 6]. Jowett published the only case with involvement of the IPJ [7].
In the case of intra-articular location, the leading symptoms are synovitis, decreased range of movement and effusion of the joint [3].
The differential diagnosis in this case included chronic inflammatory arthritis, osteochondritis dissecans, rheumatoid synovitis, tendonitis, impingement, osteoarthritis and osteomyelitis. A history of an injury can make the diagnosis of OO even more difficult. Jordan found a mean delay of 22 months between initial presentation and diagnosis [8].
Surgical excision of the nidus is still the gold standard treatment and normally resolves symptoms without recurrence if the resection of the nidus is complete. However, the use of percutaneous techniques such as CT-guided radiofrequency ablation [9] is increasing exponentially. Their results are similar to those obtained in open surgery [1], although the disadvantage is that they do not provide a definitive histologic diagnosis.
Percutaneous techniques are specially indicated for those locations where an open approach is too aggressive, like the pelvic ring or spine, considering an OO as a benign tumor [3].
In this case, we opted for an open approach because of the location of the tumor and the ease of the surgical access. However, we did not achieve the complete resection of the nidus, likely not to damage the articular surface. This lack of complete removal was the cause of recurrence.
We performed ‘in block’ excision of the lesion because the cartilage defect and the risk of articular instability, fusing the IPJ with a partial-thread screw as Jowett described [7].
Arthrodesis of the IPJ is a safe technique with excellent results and with a low rate of complications as described by Dhukaram [10]. And provides a stable lever on which the long, short flexors and extensors can function.
CONCLUSION
OO of the phalanges of the toes is rare. The diagnosis of OO when its location is intra- or juxta-articular is a challenge and often retarded because the symptoms mimic a real arthritis.
An accurate clinical history with a high index of suspicion can allow for a presumptive diagnosis to be made. Complete resection of the nidus remains decisive in order to avoid a recurrence providing immediate and permanent remission of symptoms. Although open surgery is widely used, percutaneous techniques are gaining popularity with high rate of clinical success.
Conflict of interest statement
None declared.
REFERENCES
Author notes
Deceased.



