-
PDF
- Split View
-
Views
-
Cite
Cite
Shamir O Cawich, Fawwaz Mohammed, Richard Spence, Vijay Naraynsingh, Laparoscopic removal of a gallbladder remnant in a patient with severe biliary pancreatitis, Journal of Surgical Case Reports, Volume 2016, Issue 9, September 2016, rjw163, https://doi.org/10.1093/jscr/rjw163
Close - Share Icon Share
Abstract
Many surgeons opt to perform subtotal cholecystectomy to limit duct injuries in difficult cases. In these cases, however, there is a risk for the gallbladder remnant to become diseased. In these cases, a completion cholecystectomy is necessary.
Although technically challenging, the laparoscopic approach to completion cholecystectomy is feasible and safe, when performed by surgeons with advanced laparoscopic experience.
Introduction
In difficult cholecystectomies, surgeons may perform a subtotal cholecystectomy to reduce the risk of common bile duct (CBD) injury [1]. However, the gallbladder remnant can become diseased [2] and then requires completion cholecystectomy to limit subsequent morbidity.
Although there are reports of laparoscopic completion cholecystectomies [2–9], many authorities still consider this a contraindication to the laparoscopic approach. We present one case of a completion cholecystectomy to add to the existing literature proving that the laparoscopic approach is feasible, safe and accompanied by the advantages of minimally invasive surgery.
Case Report
Three years after laparoscopic cholecystectomy, a 49-year-old woman represented with abdominal pain and vomiting. There was no history of alcohol or drug ingestion. On examination there was localized peritonitis in the epigastrium.
A diagnosis of severe biliary pancreatitis was made after investigations revealed leukocytosis (16 000/ml), hyperamylasemia (1200 U/L) and an APACHE-II score of 8. Abdominal ultrasound identified a gallbladder remnant containing multiple gallstones and a dilated CBD.
A review of hospital records confirmed elective laparoscopic cholecystectomy for biliary colic 3 years prior. The operation notes described an uncomplicated procedure with no apparent deviation from standard technique. A ‘1 × 2 × 3 cm thin-walled gallbladder with multiple stones and features of chronic cholecystitis’ was described on pathology reports. With supportive management, there was prompt resolution. The gallbladder remnant was demonstrated on MRCP (Fig. 1).
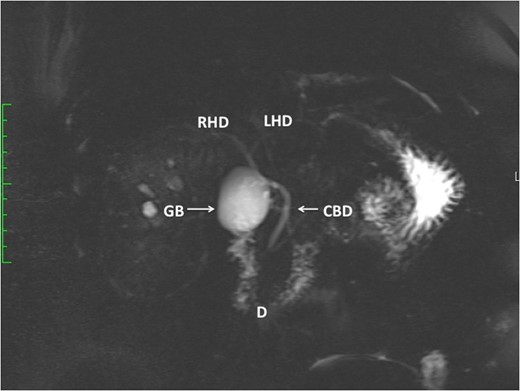
This MRCP demonstrates a large gallbladder remnant (GB). The anatomy of the duodenum (D), CBD, left (LHD) and right hepatic ducts (RHD) are normal. There are no CBD stones present.
A laparoscopic completion cholecystectomy was performed. There were multiple dense adhesions that precluded visualization of the gallbladder remnant (Fig. 2). Meticulous dissection with cautery attached to ‘hot scissors’ eventually presented the gallbladder remnant (Fig. 3). Scarring at Calot's triangle prevented retrograde dissection, so the ‘dome down’ technique was used to identify cystic duct (CD) (Fig. 4) and right hepatic structures at the floor of an open-type Rouviere's sulcus (Fig. 5). Intraoperative cholangiography was performed via the CD using a 5Fr infant feeding (Fig. 6) and confirmed that: this structure was the CD, the extra-hepatic biliary tree was normal and there were no stones in the CBD (Fig. 7). At this point, the CD and artery were ligated and ‘hot scissors’ were used to separate the gallbladder remnant from the liver bed. This patient recovered uneventfully and remained asymptomatic 2 years later.
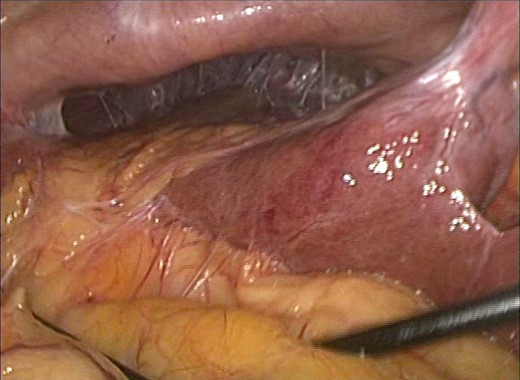
Multiple adhesions were present in the right upper quadrant preventing visualization of the gallbladder remnant.
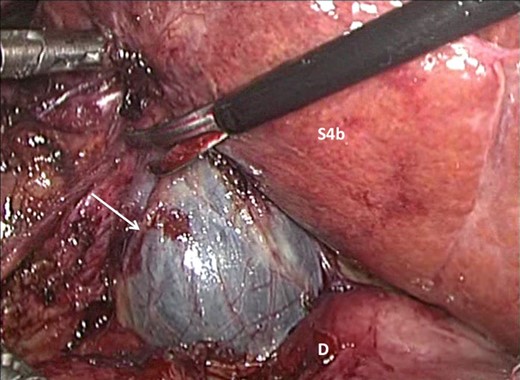
Careful dissection with ‘hot scissors’ has presented the ‘fundus’ of the gallbladder remnant (arrow). The duodenum (D) and segment IVb of the liver (s4b) are visible after dissection.
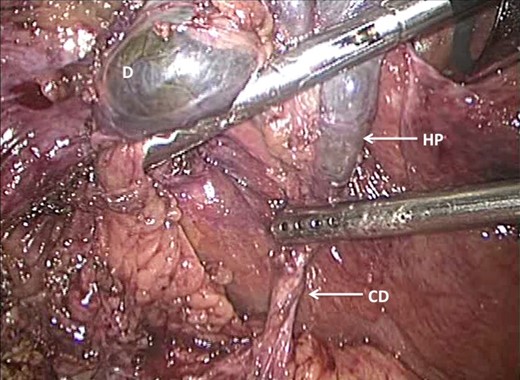
The ‘dome down’ (anterograde) dissection technique has been used to dissect from the dome (D) onto Hartmann's pouch (HP) as it tapers into the CD.
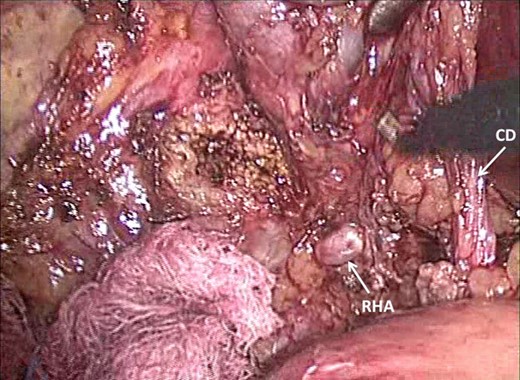
Dissection has presented Rouviere's sulcus (open-type) with the right hepatic artery (RHA) visible superficially. The close relationship to the CD in Calot's triangle is demonstrated.
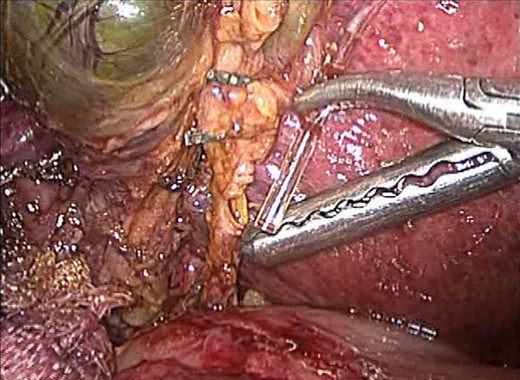
A 5 Fr infant feeding tube is fed into the opened CD in order to perform an intraoperative cholangiogram.
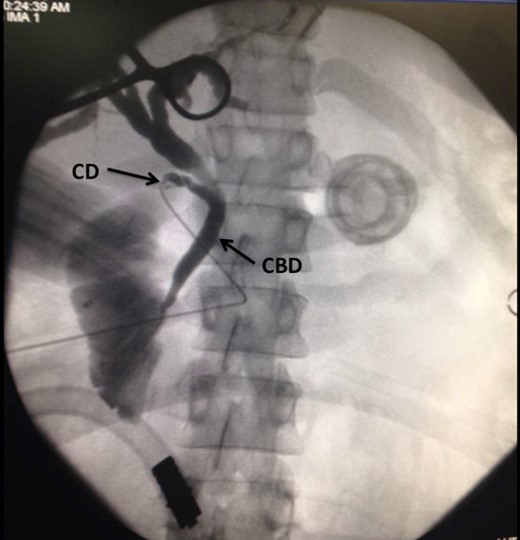
Choangiogram film demonstrating the catheter as it enters into the CD. A normal CBD is noted. There are no stones in the CBD and contrast is seen entering the duodenum.
Pathologic examination described a 2 × 3.5 cm gallbladder remnant containing multiple gallstones (Fig. 8), with changes of chronic cholecystitis.
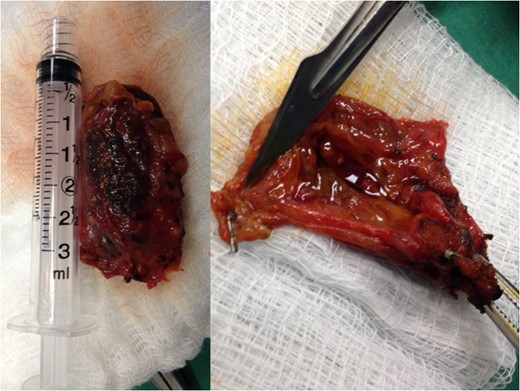
The 3.5 × 2 cm gallbladder remnant has been extracted from the abdomen. Multiple stones are seen within the remnant.
Discussion
Laparoscopic cholecystectomy is considered a basic operation that general surgeons perform routinely. In order to mitigate the risk of CBD injury, many surgeons opt to perform subtotal cholecystectomies if they encounter difficulty dissecting Calot's triangle [1].
Whether or not it is left deliberately, a gallbladder remnant may become diseased leading to Hartmann's pouch postcholecystectomy pain syndrome [2], stump cholecystitis [4, 7], biliary pancreatitis [10] or cholecysto-enteric fistulae [11]. Our patient presented with severe biliary pancreatitis—APACHE II score of 8. This is a serious consequence of a remnant gallbladder that may be accompanied by significant morbidity and mortality.
Once a symptomatic remnant is identified, completion cholecystectomy is indicated [2–7], either through an open or laparoscopic approach. Gurel et al. [12] is credited with performing the first laparoscopic completion cholecystectomy in 1995. Even though there are now several case reports [3–7] and small series [8–9] of laparoscopic completion cholecystectomies, it is still not widely accepted. We encountered one case previously in which we performed a laparoscopic completion cholecystectomy [7], but when we submitted the case for publication the reviewers’ overwhelming sentiments were that completion cholecystectomies should be performed using the open approach because the laparoscopic approach was contraindicated. This case now adds to the existing data supporting the laparoscopic approach as a feasible and safe method to perform completion cholecystectomy.
We do agree that these operations tend to be technically difficult because there is usually significant scarring and anatomic distortion at the gallbladder bed [2–9]. However, careful and patient dissection can allow the procedure to be completed safely. Even in our setting where resources are limited, we were able to perform the dissection safely using only ‘hot scissors’ without the need for ultrasonic dissectors or any specialized equipment. During dissection, it is important for the surgeon to be aware of important anatomic landmarks, such as Rouviere's sulcus. This can prevent inadvertent injury to the right hepatic pedicle structures that may present themselves in the surgical field during dissection of Calot's triangle. We also advocate dissection to approach the gallbladder remnant from the right side in order to avoid the difficult dissection near the hepatic hilum. These principles were clearly demonstrated in this case where the right hepatic structures presented themselves in the surgical field during dissection of Calot's triangle while approaching the gallbladder from its right side.
This is a complex operation and not one that should be undertaken by surgeons without advanced laparoscopic experience, and preferably under the care a hepatobiliary surgical team, who could perform specialized maneouvers for safe dissection such as the dome-down technique. We also advocate routine intraoperative cholangiography to identify critical structures during laparoscopic completion cholecystectomies. These techniques were all in use in this case and contributed to its success. Preoperative MRCP is also indispensable to plan the operative approach and to act as a ‘roadmap’ during dissection, but it cannot replace intraoperative cholangiography in our view.
Conclusion
Patients with symptomatic gallbladder remnants should be subjected to completion cholecystectomy. There is no reason to be dissuaded from performing a completion cholecystectomy laparoscopically. However, these operations are technically challenging and should be performed surgeons with advanced laparoscopic experience. Routine intraoperative cholangiography should be used to perform laparoscopic completion cholecystectomy safely.
References
Author notes
All authors contributed equally to this work



