-
PDF
- Split View
-
Views
-
Cite
Cite
Naohiro Nose, Kazuhiro Higuchi, Eiichi Chosa, Takanori Ayabe, Masaki Tomita, Kunihide Nakamura, Port-site implantation of Type A Masaoka Stage I thymoma after video-assisted thoracic surgery: a case report, Journal of Surgical Case Reports, Volume 2016, Issue 9, September 2016, rjw164, https://doi.org/10.1093/jscr/rjw164
Close - Share Icon Share
Abstract
A 60-year-old woman was referred to our hospital with an anterior mediastinal tumor measuring 3.5 cm in diameter on computed tomography (CT). We performed tumor resection by video-assisted thoracic surgery (VATS) with three ports. The final diagnosis was Type A Masaoka Stage I thymoma. On follow-up CT performed 36 months after the operation, two pleural tumors were detected at the port sites through which the forceps and ultrasonic scalpel had passed repeatedly during the operation. We therefore performed a second operation and enucleated the tumors while preserving the ribs. However, other tumor tissue was detected along the surgical marginal line during the pathological diagnosis after the operation. Surgeons should thus be aware that port-site recurrence can occur after VATS resection of Type A thymoma, despite its mild biological behavior. Wide resection of the chest wall is therefore recommended for operations of port-site recurrence after VATS thymectomy.
Introduction
Thymomas are the most common low-grade malignant tumors that often emerge in the anterior mediastinum in adults [1]. While thymectomy by sternotomy is the traditional method of treating thymoma, recently, video-assisted thoracic surgery (VATS) approaches have been often selected [2]. VATS thymectomy is reportedly feasible and safe and is less invasive than transsternal thymectomy [2, 3]. However, we experienced a rare complication of port-site recurrence that would not have occurred with transsternal thymectomy.
Case Report
A 60-year-old woman was referred to our hospital with an anterior mediastinal tumor on computed tomography (CT) performed for follow-up 6 years after a complete response to chemotherapy for malignant lymphoma. CT revealed a tumor in the right anterior mediastinum with a diameter of 3.5 cm, round shape and demarcation from the neighboring tissue (Fig. 1). No recurrent lesion of the malignant lymphoma was detected. She had no symptoms, including none due to myasthenia gravis. Her anti-acetylcholine receptor antibody level was 0.2 nmol/L (within normal range). To confirm the diagnosis and treat the patient, we planned tumor resection via VATS.
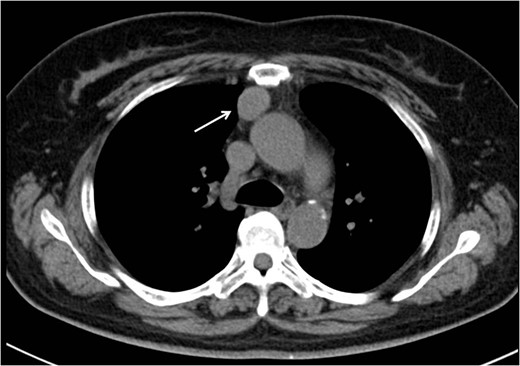
Initial CT revealed a tumor in the right anterior mediastinum with a diameter of 3.5 cm, round shape, which was clearly demarcated from the neighboring tissue.
The operation was performed with three thoraco-ports in the spine posture. The first 15-mm thoraco-port for the videoscope was placed in the sixth intercostal space on the mid-axillary line. There was no adhesion or disseminated lesions in the thoracic cavity. The second 15-mm port was placed on the fifth intercostal space on the anterior axillary line. The third 5-mm port was placed in the fourth intercostal space on the anterior axillary line. The tumor was easily identified under the mediastinal pleura as an elevated mass in the thymic tissue. Through the second and third ports, thymectomy was performed. The normal thymus around the tumor was grasped by forceps and cut using an ultrasonic scalpel with marginal tissues. After the resected tumor was placed into a specimen bag, it was removed through the second port. We did not detect any breakage of the tumor during the surgery. Frozen sections during the operation revealed that the tumor was capsulated Type A Masaoka Stage I thymoma with sufficient marginal tissue. This diagnosis was also verified using a fixed permanent specimen.
Follow-up CT performed 36 months after the operation revealed two pleural tumors located near the second and third ports (Fig. 2a and b). We suspected the pleural recurrence of thymoma and performed a second operation. Initially, the operation was performed only by VATS with three ports. After removing the severe adhesion between the lung and chest wall, we were able to identify the two tumors. As with the extrapleural tumor, the tumors arose from the intercostal space. Their surfaces were covered with parietal pleura with partial irregularity (Fig. 3). There were no other recurrent findings in the thoracic cavity. Given these findings, we diagnosed these tumors as port-site implantations after the first VATS.
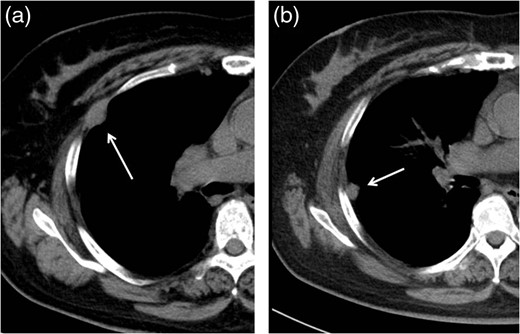
Follow-up CT at 36 months after the operation revealed two pleural tumors locating at the second (a) and third (b) ports used in the VATS operation.
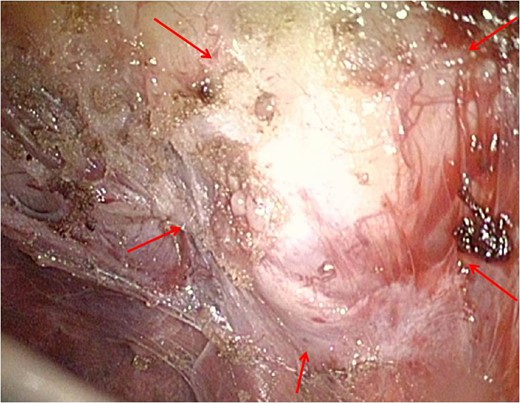
In the operative findings, the tumors were found to have arisen from the intercostal space, and their surfaces were covered with parietal pleura with partial irregularity.
With no definitive findings suggesting tumor invasion into the rib, we decided to resect the tumors while preserving the ribs. We performed mini-thoracotomies just above the tumors and enucleated those two tumors via the mini-thoracotomies using an electric scalpel. To obtain a sufficient surgical margin, we visualized the adequate resected line using a thoracoscope while cutting the intercostal tissue surrounding the tumor. The pathological diagnosis was Type A thymoma, which was consistent with port-site metastasis of the initial tumor. The surgical margins of both tumors were positive, indicating incomplete resection. After relating these findings and the incomplete resection to the patient, we decided on close follow-up without reoperation.
Discussion
Port-site recurrence after VATS for thymoma is rare. Ishibashi et al. reported a case of port-site recurrence after a VATS operation for Type B2 thymoma [4], to our knowledge, this is the only such previous case report. The current Type A and the reported Type B2 thymomas are low-grade malignant tumors. Despite their mild biological behavior, implantation at the port-site still occurred. Cases of implantation after medical procedures have been reported, not only for malignant tumors, but also for benign tumors [5]. Surgeons should thus be aware that port-site implantation can occur regardless of the tumor's malignant potential.
The mechanism of port-site recurrence is unclear. Willard et al. [6] reported a case that recurred in the small VATS port through which partially resected lung cancer had been extracted without a specimen bag. In our case, the implantation developed only at the second and third ports, through which the forceps and ultrasonic scalpel had passed repeatedly. Although we did not detect any tumor exposure during the first operation, we cannot help but assume that the implantation occurred due to contamination with tumor cells from either the ultrasonic scalpel or forceps that had grasped tissue near the tumor. Of further note, implantation did not develop in other pleura in which tumor tissue must surely have been disseminated by contaminated equipment. Taken together, these findings suggest that one of the possible causes of port-site implantation was the rubbing of tumor cells, such as thymoma, which might have a high affinity for pleura [5], against the VATS ports. Surgeons should take extreme care to grasp the tissue as far as possible from the tumor and to use a specimen bag even when tumor exposure is not recognized.
We were unable to achieve complete resection in the second operation. Given the lack of any definitive clinical findings that the tumors had invaded the neighbor ribs, we believed that the tumors could be enucleated completely while preserving the ribs. However, the enucleation of the tumors located mainly in the narrow intercostal spaces with a sufficient margin was very difficult. Although no definitive tumor invasion to the skin or subcutaneous tissue was identified, they might nevertheless invade the ribs pathologically. Ishibashi et al. [4] successfully performed a curative operation in a case of port-site recurrence via wide chest wall resection and reconstruction. In the process, they proved the presence of pathological tumor invasion to neighboring ribs. A small-extent resection of the skin and wide resection of the chest wall is therefore recommended when performing surgery for port-site recurrence after VATS thymectomy.
CONFLICT OF INTEREST STATEMENT
None declared.



