-
PDF
- Split View
-
Views
-
Cite
Cite
Savino Occhionorelli, Ilaria Pigato, Enzo Malvicini, Giovanni Pascale, Rocco Stano, Rosa Rinaldi, Giorgio Vasquez, Solitary fibrous tumour of gluteus: a case report about an uncommon localization of a rare neoplasm, Journal of Surgical Case Reports, Volume 2016, Issue 6, June 2016, rjw111, https://doi.org/10.1093/jscr/rjw111
Close - Share Icon Share
Abstract
Solitary fibrous tumour (SFT) is a rare benign tumour that occurs most frequently in the pleura. It is considered rare in soft tissues. We report a case of a middle-aged woman that presented a solitary fibrous tumor of gluteus. The tumour was composed of mesenchymal spindle-shaped cells positive for CD34 and bcl-2. Although rare, SFT should be included in the differential diagnosis of mesenchymal soft tissue tumours. The clinical presentation and imaging can be helpful for a better pre-operative diagnosis.
INTRODUCTION
Solitary fibrous tumour (SFT) is a rare mesenchymal neoplasm, first described in 1931 by Klempere and Robin in a patient with a distinctive pleural lesion as a mesothelial tumour arising from the pleura [1]. SFT is distinguished into two entities, pleural and extra pleural. In the thoracic cavity, they are usually asymptomatic and discovered incidentally on a routine X-ray of the chest or during check-up for other abnormalities. Extra pleural SFTs are observed in middle-aged adults (median age 50 years) and affect both sexes equally (male:female = 1:1.2). In recent years, increased interests for this type of tumour led to its recognition in a large number of extra thoracic sites, including the meninges, orbit, upper respiratory tract, salivary glands, thyroid, peritoneum, liver, retro-peritoneum and pelvis, adrenal gland, kidney, spermatic cord, urinary bladder, prostate, uterine cervix, spinal cord, periosteum and soft tissues [2]. Extra thoracic SFTs are rare and account approximately 0.6% of all soft tissues tumours [3]. Clinically, it is generally a slow-growing, painless, well-delineated exophytic mass; large tumours can cause compressive symptoms and rarely paraneoplastic syndromes (i.e. hypoglycemia secondary to insulin-like growth factor). The dimensions of SFT can vary from 1 to 25 cm in diameter.
Like pleural SFTs, extra-thoracic SFTs usually have a benign prognosis, however, a small number of cases with atypical histological features has been reported to develop local recurrence or metastasis [4].
CASE REPORT
In July 2007, a 63-year-old white woman referred to a first-level Hospital for a palpable lesion in correspondence of right gluteus. She had not fever neither pain, but only a swollen area in perianal region. She was submitted to Ultrasounds (US), that showed an hypervascularized swelling that was interpreted as a voluminous hematoma (size 13 × 10 cm, thickness 4–5 cm), partially organized in the context of muscular structures of right gluteus (Fig. 1). After antibiotic therapy without any size regression, the patient was submitted to a Computed Tomography (CT) of abdomen and pelvis.
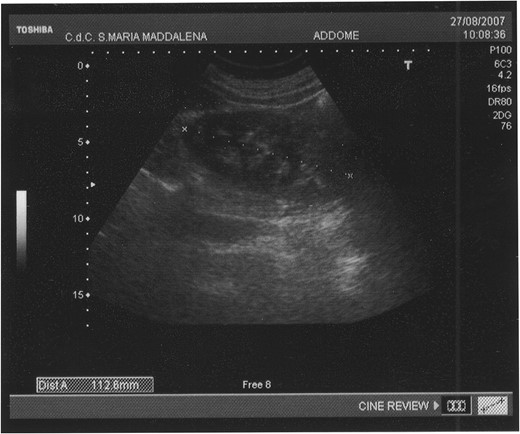
The abdominal ultrasound (US) shows an ovoid swelling, misinterpreted as a partially organized hematoma in the contest of the right gluteus maximus muscle.
CT showed an hyperintense and inhomogeneous solid lesion taking up the right ischiorectal fossa (maximum diameter of about 10 cm), extended cranially until impressing the wall of the rectal ampulla, with no apparent infiltration (Figs 2 and 3). The lesion presented an intense contrast enhancement, sign of a rich vascularization (Fig. 4).
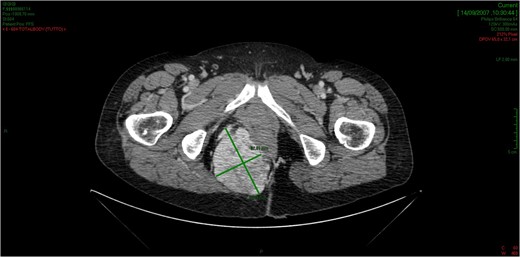
The CT scan demonstrates a solid neoformation in the right ischiorectal fossa.
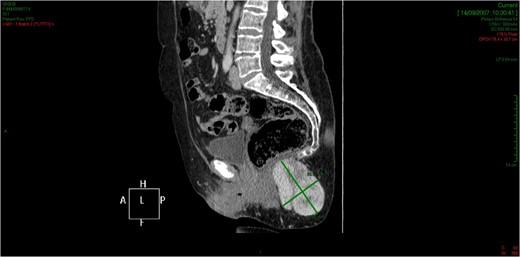
The lesion extends cranially until impressing the wall of the rectal ampulla, with no apparent infiltration.

The tridimensional reconstruction shows the rich vascularization of the neoplasm.
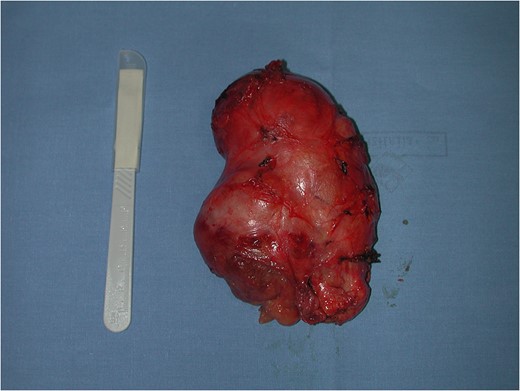
Surgical treatment was carried out with a posterior approach (Fig. 5). The lesion was in close proximity of elevator ani muscle and lateral rectal wall, that were not macroscopically infiltrated. The lesion area was marked with surgical clips because of the close proximity with rectal wall, for eventual post-operative chemotherapy or radiotherapy and for follow-up. Surgical specimen was an oval, soft tissue mass of 11 × 7.5 × 5.5 cm in size, capsulated, hyper-vascularized, with a inhomogeneous aspect, multi-lobed (Fig. 6). Microscopically, the tumour was composed by a proliferation of spindle cells crossed by stromal collagen and giant plurinucleate cells. Neoplastic cells immunophenotype showed expression for CD34 and bcl-2 (Figs 7–9).
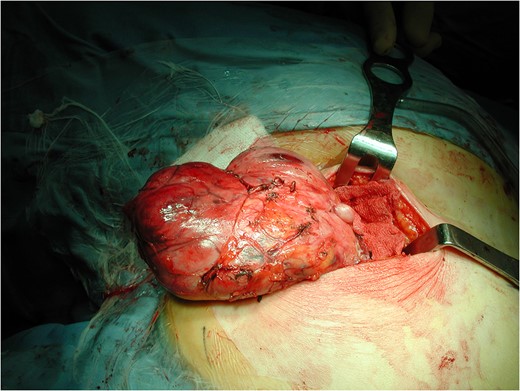
Posterior surgical approach and intra-operatory appearance of the neoplasm.
Variable cellularity and vascular patterns hemangiopericitoma-like in solitary fibrous tumour.
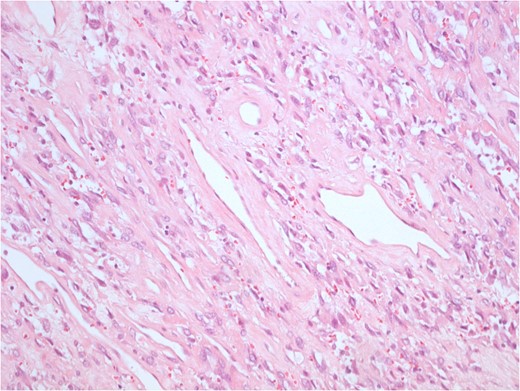
Uniform spindled cells in variably collagenous and vascular pattern. The tumour cells form random and trabecular arrangements.
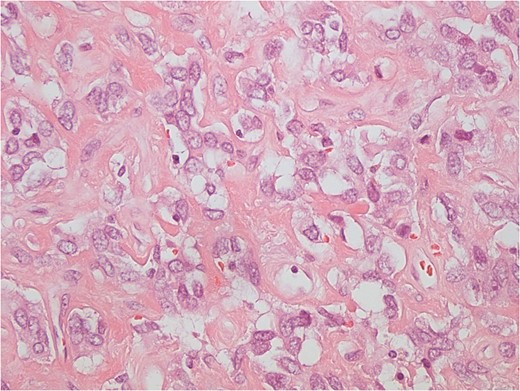
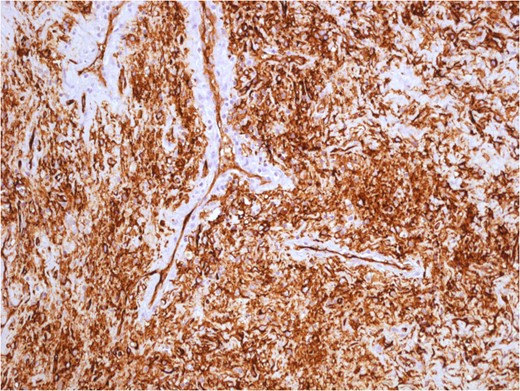
The tumour cells have indistinct cytoplasm and oval nuclei, with inconspicuous nucleoli. Collagenous background is evident. Mitotic activity is absent. SPT cells are positive for BCL2 and CD34.
The patient was discharged home on fifth post-operative day, and she did not receive any further therapy. In December 2008, she presented an hypo-dermal recurrence in the same area demonstrated with CT-scan (Fig. 10). The patient underwent to surgery for complete resection of the recurrent lesion. After 1 year, a Magnetic Resonance (MRI) demonstrated the surgical scar without sign of recurrence. After a 7-years follow-up the patient is still alive, without any clinical or radiological evidence of recurrence, she did not need any chemotherapeutic or radiotherapeutic treatment.

The CT scan demonstrates an hypodermal recurrence of the lesion in the side of resection marked with a metallic clip.
DISCUSSION
The histological appearance of SFTs may overlap with other benign and malignant diagnostic entities, such as hemangiopericytoma, leiomyoma, nodular fasciitis, inflammatory myofibroblastic tumour, fibromatosis and benign peripheral nerve sheet tumour [5]. In the past, SFTs were considered rare tumours originated from mesothelial cells. This has been recently proved using immunohistochemical analysis, particularly positive staining for CD34 and bcl-2 is an indication of SFT [5]. Usually, microscopic features are the presence of relatively spindled cell set in variably collagenous, cellular and in some cases myxoid matrix. An hemangiopericitoma-like vascular pattern in seen at least focally in most cases. Tumour cells have indistinct cytoplasm and oval nuclei, with inconspicuous nucleoli. Mitotic activity is low (<2–3 mitoses/10 HPF, high-power fields) in most cases, but some tumours show overtly sarcomatous features with a high mitotic activity.
SFTs are aggressive in 10–15% of cases. Malignant SFTs are characterized by large tumour size (more than 50 mm), infiltrative margins, greater cellularity with an infiltrative growth pattern, moderate to marked cellular atypia, and high mitotic activity (>4 mitotic cells/10 HPF, high-power fields) [5, 6].
The tumour is difficult to detect because it has no typical radiologic features: on X-ray it appears as a moderately radio-opaque mass, on US as a nodule with generally well-defined borders and an homogenous echo-structure. However, clinical findings, MRI and US are not sufficient for a definitive diagnosis.
In this case report, the lesion appears like a voluminous hyper-vascularized hematoma, but patient's anamnesis was negative for traumatic events. Patient's anamnesis took distant from an inflammatory process, because the patient had not fever or leukocytosis. CT scan and MRI usually reveal a well defined capsule surrounding an homogenous mass with progressive enhancement from the arterial to venous phase and occasionally multiple small non-enhancing portions [7]. Positron emission tomography (PET) may be helpful to distinguish between a malignant and a benign variant of the tumour [8], but the gold standard for diagnosis remains the incisional biopsy.
The clinical behavior of SFTs is unpredictable [9]. The relationship between morphology and outcome is poor. Most of SFTs are characterized by non-aggressive clinical course. Systemic symptoms such as hypoglycemia, arthralgia, osteoarthritis and clubbing have also been reported. Lesions located in mediastinum, abdomen, pelvis or retroperitoneum are usually more aggressive than those in the limbs. Metastases are most often reported in the lungs, bone and liver.
Surgery is considered the first choice of treatment and the use of chemotherapy is reserved to metastatic or symptomatic and non-resectable SFTs, but there are no standard chemotherapeutic regimens. Generally, to avoid recurrences a local wide resection of these tumours may be recommended. Radiation therapy has some benefit in combination with chemotherapy [10].
CONFLICT OF INTEREST STATEMENT
None Declared.



