-
PDF
- Split View
-
Views
-
Cite
Cite
Tatiana Santos, Carla Freitas, João Pinto-de-Sousa, Gastric wall ischemia following massive gastric distension due to peptic pyloric stenosis: a case report, Journal of Surgical Case Reports, Volume 2016, Issue 2, February 2016, rjw008, https://doi.org/10.1093/jscr/rjw008
Close - Share Icon Share
Abstract
Gastric necrosis is a rare entity mainly due to the rich collateral blood flow the stomach is supplied by. Acute gastric dilation is one of the described underlying causes, and although not fully understood, many potential alterations, such as vascular compression, herniation, volvulus, acute necrotizing gastritis, complications after abdominal surgery, anorexia, bulimia nervosa, trauma, exposure to caustic materials, diabetes, medications, infections, debilitating chronic illness, gastric outlet obstruction, aerophagia and acute pancreatitis have been described. In this report, we present a case of partial gastric ischemia with necrosis and consequent perforation of the lesser curvature of the stomach, as a result of gastric outlet obstruction due to pyloric stenosis. The patient underwent an emergency laparotomy. An atypical gastrectomy and a Heineke–Mikulicz pyloroplasty were performed. We emphasize the need for the quick recognition of this condition and for the urgent management because of the high mortality rate associated with undiagnosed gastric necrosis.
INTRODUCTION
Gastric ischemia and necrosis is an uncommon event mainly due to the rich collateral blood flow the stomach is provided with [1, 2]. In the very few cases reported in the literature, a number of etiological factors have been proposed, such as intrathoracic herniation of the stomach, volvulus, acute necrotizing gastritis, vascular compromise and acute gastric dilation [3].
Acute gastric dilation can be due to diverse factors such as vascular compression, herniation, volvulus, complications after abdominal surgery, anorexia, bulimia nervosa, trauma, exposure to caustic materials, diabetes, medications, infections, debilitating chronic illness, gastric outlet obstruction and even aerophagia [3, 4]. Gastric wall ischemia is expected to occur if the increase in the intragastric pressure eventually results in impaired intramural blood flow [1]. It has been described that pressures higher than 14 mmHg can cause impairment of mural venous blood flow, which corresponds to an intraluminal quantity of >3 l of fluid [2, 5]. Acute gastric dilation is believed to occur mostly in women, and ischemia is more frequently found in the lesser curvature of the stomach because of the poorer local vascular supply [1].
According to the few cases reported so far, the high mortality (50–80%) associated with this condition imposes an emergent surgical approach. In most cases, decompression and surgical resection of the affected portion of the stomach is the usual procedure to adopt [2, 3].
Herein, we present a case of a gastric partial necrosis with perforation following massive gastric dilation secondary to gastric outlet obstruction due to unrecogized peptic stenosis. Although an underlying chronic degree of gastric dilation was certainly present, due to the nature of the obstruction, we believe that an acute gastric distension leads to the development of ischemia.
CASE REPORT
An 85-year-old woman with a previous history of long-term peptic ulcer, under proton pump inhibitor therapy, and hypertensive arterial disease, was admitted to our emergency department with complaints of abdominal distension, upper abdominal pain and alimentary vomit for the last 12 h.
On physical examination, she had tenderness and guarding in all abdominal quadrants. All vital signs were within normal range. The laboratorial tests revealed only a mild increase in systemic inflammatory parameters but with no organ failure.
The patient underwent an abdominal plain film, which identified a massive gastric dilation and a pneumoperitoneum was suspected (Fig. 1). In order to confirm these findings, an abdominal computed tomography (CT) was performed, which clearly identified a massive gastric dilation. The stomach reached the pelvis and had an abrupt stricture at the level of the pylorus. A large pneumoperitoneum was also confirmed (Fig. 2).
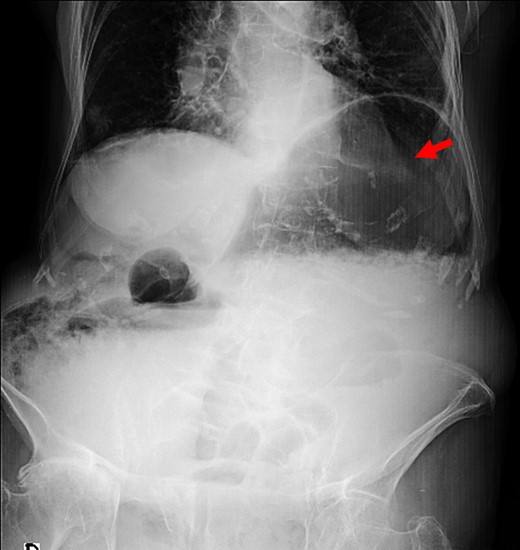
Plain abdominal film with massive gastric distension (red arrow).
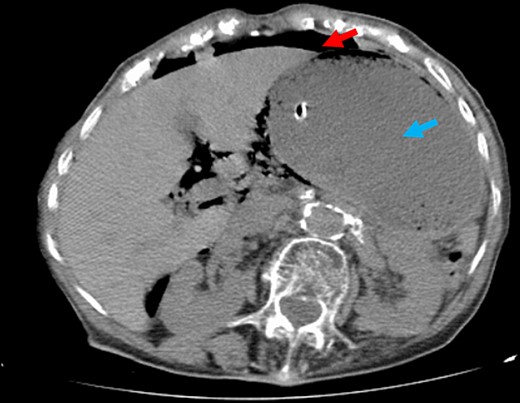
Abdominal CT. Note the large volume pneumoperitoneum (red arrows) and exuberant gastric dilation (blue arrows).
An urgent laparotomy was performed, and intraoperatively an exuberant gastric dilation was detected, with only a small amount of seropurulent free peritoneal fluid. On abdominal exploration, a limited area of necrosis with ∼2 cm was detected in the lesser curvature of the stomach. After inspection, an anterior gastrotomy was performed to empty the stomach (a total of 4 l of fluid was aspirated) and to access the area of mucosal necrosis. At last, an affected area of 3 cm × 2 cm close to the lesser curvature was identified, and an atypical gastrectomy was performed, using a linear stapler. An underlying pyloric stenosis was identified, which was circular and that seemed not to be malignant. Therefore, a Heineke–Mikulicz pyloroplasty was performed besides the partial gastrectomy. During the surgery, it was decided not to perform a vagotomy, considering the patient age and to prevent gastric emptying impairment in a patient who had already a certain degree of gastroparesis.
The postoperative period was event free, and the patient was discharged home at Day 9 after surgery. On the first postoperative evaluation, 1 month after discharge, the patient was symptoms free, namely without complaints of nausea, vomit or postprandial fullness. The pathological examination of the surgical specimen revealed gastritis with necrosis and perforation, but no malignancy was identified.
DISCUSSION
After its first description by Duplay in 1833, diverse etiologies have been proposed to explain the development of acute gastric dilation [6]. However, to the best of our knowledge, no single association has been convincingly linked to this clinical entity.
Gastric necrosis from acute gastric dilation is a rare but life-threatening condition, which requires quick diagnosis and management. After initial stabilization, surgery with resection of the affected area is the mainstay for treatment. During the surgery, a gastrotomy should be performed in order to access the true extent of the ischemia since it has been described that ischemia of gastric wall initially causes mucosal necrosis which develops before the full-thickness gastric wall necrosis [7]. Indeed, the outlayer view of the gastric wall might not correlate well with the true amount of involved portion of the stomach.
Most of the cases reported in the literature describe the need for total gastrectomy because of the extent of gastric necrosis. In the present case, the gastric necrosis was limited to a small portion of the lesser curvature, and therefore a more conservative approach was possible. Our patient had a previous history of peptic disease with pyloric stenosis that led to the massive gastric dilation caused by gastric outlet obstruction, and therefore, the subsequent ischemia and necrosis of the gastric wall arose. Probably, the chronic degree of dilatation that the stomach had previously to this acute episode contributed to the limited ischemic area.
Additionally, because of the patient's age, the vasculopathy present in gastric blood vessels might also have played a role in the pathogenesis of the ischemia.
This report documents the successful management of a rare surgical condition. Nevertheless being a potential lethal condition, its prompt identification and the immediate surgical management can offer the patient a chance to survive.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- pancreatitis, acute
- ischemia
- anorexia nervosa
- diabetes mellitus
- vascular flow
- diabetes mellitus, type 2
- bulimia nervosa
- gastrectomy
- aerophagy
- caustics
- chronic disease
- dilatation, pathologic
- hernias
- laparotomy
- mikulicz disease
- necrosis
- gastric dilatation
- wounds and injuries
- infections
- pyloric stenosis
- gastric outlet obstruction
- mortality
- stomach
- intestinal volvulus
- abdominal surgery
- pyloroplasty
- loss of appetite
- stomach wall
- undiagnosed
- vascular compression
- necrotizing gastritis
- gastric ischemia



