-
PDF
- Split View
-
Views
-
Cite
Cite
Pedro N. Brandão, Isabel Mesquita, Mónica Sampaio, Pedro Martins, Jorge Daniel, José Davide, Foramen of Winslow hernia: case report of a minimally invasive approach, Journal of Surgical Case Reports, Volume 2016, Issue 12, 1 December 2016, rjw205, https://doi.org/10.1093/jscr/rjw205
Close - Share Icon Share
Abstract
Foramen of Winslow hernias account for 8% of all internal hernias. Their non-specific presentation and often late diagnosis are associated with an estimated mortality of 50%. The use of complementary diagnostic methods facilitates the diagnosis and planning of the therapeutic strategy. Urgent surgery is the appropriate treatment due to the risk of intestinal ischemia, being laparotomy the main form of approach described. Few cases of laparoscopy are referred to in the literature.
Introduction
An internal hernia is defined as the protrusion of visceral contents through a congenital or acquired foramen within the limits of the peritoneal cavity [1].
The foramen of Winslow hernia accounts for 0.08% of all hernias and 8% of all cases of internal hernias [1, 2]. It is located beneath the free edge of the lesser omentum and the hepatoduodenal ligament. The posterior, superior and inferior limits include the inferior vena cava, caudate lobe and duodenum, respectively [2].
The small bowel is the most frequently involved organ, followed by the cecum, the ascending colon and the transverse colon. Included among predisposing factors are a wide epiploic foramen, a redundant colon, the absence of peritoneal fixation of the colon, etc. [1].
The non-specific and indolent clinical symptoms and signs cause challenging situations in terms of diagnosis. It is estimated that in only ~10% of the cases, a proper diagnosis is preoperatively established [3]. Characteristic symptoms of intestinal obstruction are often present, however, other clinical manifestations may occur. A late diagnosis is associated with a high mortality rate, estimated at ~50%. The use of complementary diagnostic procedures such as the computed tomography (CT) allows a proper evaluation and diagnosis in many cases.
The treatment requires urgent surgical approach, aiming the reduction of the herniated content. Surgical resection is meant for cases of irreversible ischemia. About seven cases of laparoscopic approach have been reported to date [2].
Case Report
A 42-year-old woman with no relevant medical history, presented at the Emergency Department with epigastric pain, of sudden beginning and progressive worsening, with a few hours of evolution. Mild abdominal distension and pain on palpation were noted, but there were no signs of peritoneal irritation. An increase of pancreatic enzymes (amylase: 201 U/L and lipase: 880 U/L) was observed and recorded as abnormal finding. As there was diagnostic uncertainty and no obvious cause for acute pancreatitis, an abdominal-pelvic CT was performed. It reported the presence of an interposition of the transverse colon between the left lobe of the liver and the stomach, probably related to a foramen of Winslow hernia. There was no pneumoperitoneum. Only a small quantity of free liquid was observed.
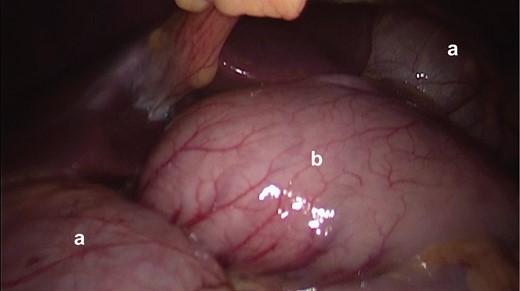
Initial picture in diagnostic laparoscopy. It is seen that the herniated colon (a), through the foramen of Winslow and the stomach (b).

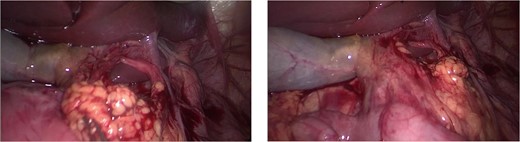
Hepatoduodenal ligament, with visualization of the herniated colon (a) and mesocolon in torsion.
The postoperative care progressed favorably without complications. The diet was started on the first postoperative day, being the intestinal transit restored. The patient was discharged on the third day after surgery. After 15 months of follow-up, the patient was asymptomatic and there was no evidence of recurrence.
Discussion
Since the first publication by Blandin in 1834, <200 cases of foramen of Winslow hernias have been reported in medical literature [4].
Their rarity and non-specific presentation make diagnosis a challenge. In rarer cases, where abnormal findings such as the elevation of pancreatic enzymes are observed, it is even more difficult to interpret the clinical picture and obtain an appropriate strategy for diagnosis and treatment.
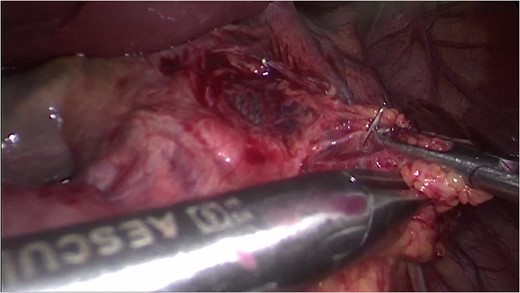
The use of complementary diagnostic methods, such as the CT, enables the surgeon to establish a proper diagnosis and consider a laparoscopic approach, in due time. A thorough examination of the entire abdominal cavity is required to assess the viability of the herniated content. In most situations it is possible to reduce the contents, however, cases of needle decompression are described as an adjuvant procedure in this process [2]. Intestinal resection is meant for cases of irreversible intestinal ischemia. The closure of the foramen is controversial since there is no consensus among the different authors [3].
In summary, despite the advances in imaging methods, the identification of the foramen of Winslow hernia remains difficult due to its rarity and non-specific form of presentation. The laparoscopic approach should be considered as an effective alternative allowing a minimally invasive way to achieve definitive treatment.
Conflict of Interest Statement
None declared.



