-
PDF
- Split View
-
Views
-
Cite
Cite
Natasha Hansraj, Shannon M. Larabee, Kimberly M. Lumpkins, Anomalous mesenteric vessel—a rare etiology of intermittent partial small bowel obstruction, Journal of Surgical Case Reports, Volume 2016, Issue 12, 1 December 2016, rjw209, https://doi.org/10.1093/jscr/rjw209
Close - Share Icon Share
Abstract
We report a case of an 11-year with recurrent episodes of abdominal pain and vomiting. Diagnostic laparoscopy during a severe episode demonstrated an anomalous blood vessel incompletely encircling the bowel, leading to transient partial small bowel obstruction. This likely represents a remnant vessel from the omphalomesenteric duct. Recurrent abdominal pain and vomiting in the pediatric population requires careful history and physical exam, and a willingness to entertain unusual diagnoses.
INTRODUCTION
Recurrent abdominal pain (RAP) is a common pediatric condition, with more than one-third of the elementary and middle school children complaining of weekly abdominal pain [1]. Organic causes are noted in 8–45% of patients with RAP [2]. Surgical causes are uncommon and typically include biliary dyskinesia or malrotation. We present an 11-year girl with recurrent bouts of abdominal pain and nausea caused by a partial small bowel obstruction (pSBO) due to an aberrant blood vessel.
CASE REPORT
An 11-year-old Caucasian girl presented to the emergency room with acute abdominal pain and emesis for 24 hours. The patient had a history of three prior episodes of intermittent colicky periumbilical pain and non-bilious emesis within the preceding 5 months, each of which resolved within 1 day. She had no weight loss, food aversion, constipation or other intercurrent gastrointestinal symptoms. She was being evaluated ‘as an outpatient’ for cyclical vomiting. Sixteen hours prior to presentation she was noted to have progressive onset of periumbilical pain with multiple episodes of non-bilious non-bloody emesis, consistent with her previous attacks. However, this episode was far more severe, triggering presentation to the emergency room. She was noted to have obstipation since the onset of symptoms. No family history of Crohn's disease was identified.
On presentation, the patient was a hemodynamically stable thin girl, who was afebrile and with normal vital signs. On examination, she was noted to have periumbilical tenderness and moderate distention. Laboratory values were significant for leukocytosis to 16.3, normal hemoglobin, albumin, bicarbonate, CRP and urinalysis. An ultrasound was performed at the referring hospital, which was unable to visualize the appendix. A subsequent CT scan was notable for a normal appendix, mild wall thickening of the distal ileum and distended small bowel with associated edema. Given the evidence of SBO and concern for terminal ileitis, the patient underwent nasogastric decompression and transfer to the tertiary care children's hospital for evaluation for Crohn's disease. Magnetic resonance enterography, however, demonstrated normal terminal ileum with moderately dilated small bowel loops consistent with mild pSBO.
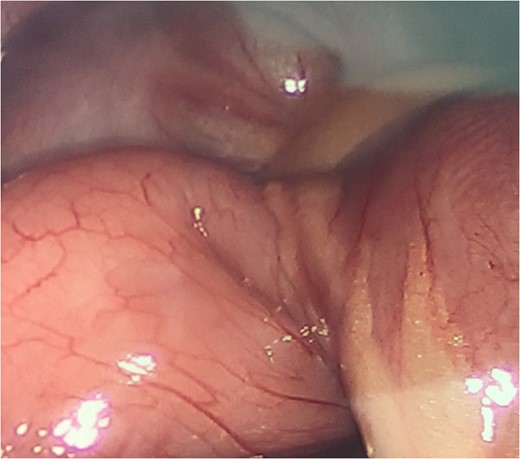
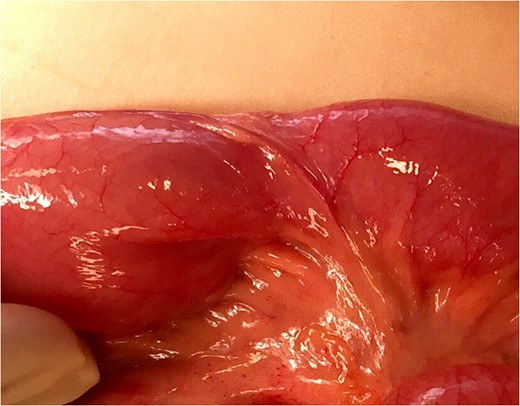
Laparoscopic view of anomalous vessel with relative constriction of the bowel.
DISCUSSION
RAP or abdominal migraine is defined by the Rome III criteria as paroxysmal episodes of intense acute periumbilical pain lasting for hours with periods of usual intervening health. Pain is associated with nausea, vomiting, anorexia, pallor or headaches without evidence of inflammatory, anatomic, metabolic or neoplastic processes. A similar description has been established by the international classification of headache disorders (ICHD-2) [3]. A related condition is cyclic vomiting syndrome, consisting of episodic, recurrent bouts of vomiting with no trigger that causes symptoms of listlessness, nausea, anorexia and abdominal pain that often require IV rehydration. A family history of migraines is often found, with children frequently transitioning from cyclic vomiting syndrome to migraine headache around adolescence [4].
When diagnosing abdominal migraine or cyclic vomiting syndrome, care must be taken to evaluate for more worrisome abdominal symptoms including abdominal distension, or worsening abdominal tenderness, neurologic signs of increased cranial pressure and worsening of symptoms [4]. Although most children with RAP or cyclical vomiting do not have an anatomic cause, this case demonstrates the importance of evaluating for rare etiologies. This patient had recurrent bouts of pain and vomiting before the true diagnosis of intermittent pSBO was made. In the pediatric patient, the leading causes of primary SBO in the virgin abdomen are related to Meckel's diverticula and congenital bands [5]. Various case reports have demonstrated the presence of an anomalous band occurring between intestinal segments, liver and intestines or abdominal wall or even from the antimesenteric wall of the intestines to the root of the mesentery. These bands can cause extrinsic compression or entrapment of bowel. This can be intermittent due to twisting and untwisting of bowel around the band [6–10]. Management can be laparoscopic or open ligation of the band.
This presentation of an anomalous vessel running from the mesenteric border to and beyond the antimesenteric border of the intestine without a corresponding adhesive band represents a very rare cause of SBO. Given the anatomic location of the vessel, it likely represents a remnant of the omphalomesenteric duct. Although the blood vessel was not part of a fibrous band, the vessel was not distensible like the intestinal wall. Presumably under normal circumstances, this vessel was non-obstructive. When the small bowel geometry became unfavorable ‘due to intermittent kinking during peristalsis’, the vessel prevented dilation of 70% of the lumen, potentially leading to increased proximal bowel dilatation and worse kinking of the bowel. This would resolve spontaneously with emesis or ‘further’ peristalsis.It is difficult to fully explain why this first presented at such a late age. It is possible that there was differential growth of the bowel and blood vessel over time, leading to an increasing mismatch between bowel diameter and the non-distensible blood vessel. This anomalous blood vessel could not be identified by radiologic studies and highlights the importance of considering surgical etiologies for unusual presentations of RAP and vomiting.
Conflict of interest statement
None declared.



