-
PDF
- Split View
-
Views
-
Cite
Cite
Ana Lopez-Marco, Naail Al-Zuhir, Malgorzata Kornaszewska, Ectopic intrapleural thymoma: a rare location in the thoracic cavity, Journal of Surgical Case Reports, Volume 2016, Issue 1, January 2016, rjv166, https://doi.org/10.1093/jscr/rjv166
Close - Share Icon Share
Abstract
We present a patient with a large thymoma on the right thoracic cavity developing from the visceral pleura. This is a rare location for this tumour, and only a few had been reported to date in the literature.
INTRODUCTION
Thymomas are rare tumours originating from the thymic epithelium. They account of the 1% of the adult neoplasms and are the most frequent anterior mediastinal tumours [1, 2].
Ectopic thymomas originate from aberrant embryological migration of thymic tissue. The most common locations for these ectopic thymomas are the neck, middle and posterior mediastinum and lung. The pleural location is extremely rare and has been documented only a few times [3–6].
CASE REPORT
A 57-year-old man presented with symptoms of chest infection and shortness of breath. After a course of antibiotics, the infection resolved, but he remained extremely short of breath.
A chest X-ray showed elevation of the right hemidiaphragm, and therefore a computed tomography (CT) scan was performed, demonstrating a 15 cm right-sided lower intrapleural mass.
A CT-guided thoracic biopsy was performed showing a cellular tumour with ovoid cells, prominent vasculature and small lymphoid cell infiltrate (Fig. 1).The immunohistochemistry analysis revealed that the ovoid cells were positive for epithelial keratin (AE1/AE3), bcl-2, CD20 and negative for CD34. The lymphoid component was positive for CD3, Tdt, CD99, Ki67 and bcl-2. Given these histopathologic features, the tumour was diagnosed as a type B thymoma according to the World Health Organization (WHO) classification.
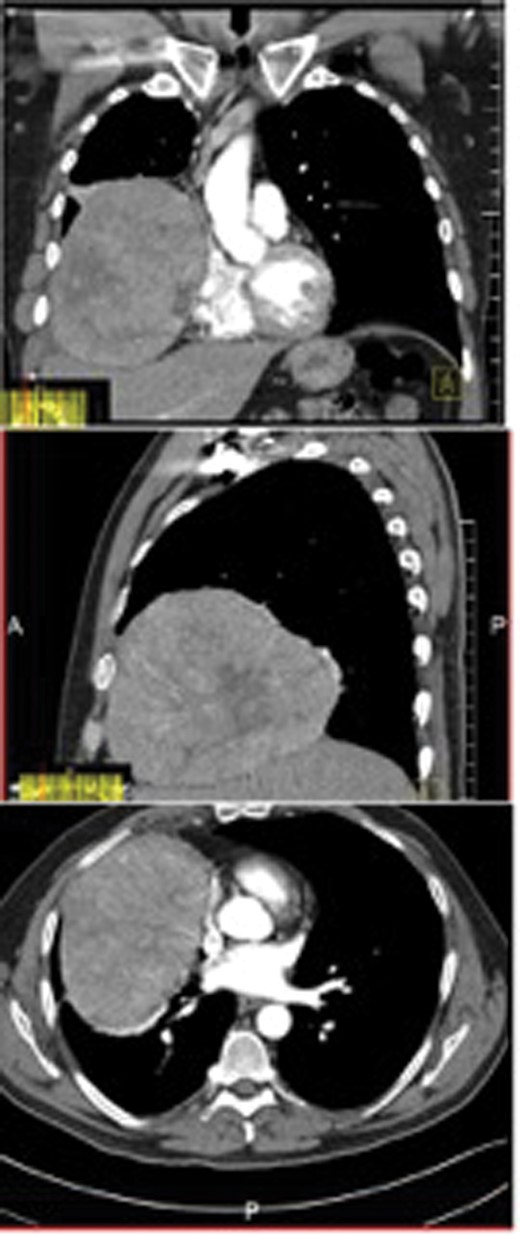
Coronal, sagittal and axial views of the CT scan showing a 15 cm intrapleural mass in the right lower chest cavity.
Surgical resection was performed with general anaesthesia and single lung ventilation via a right anterolateral thoracotomy. A 15 × 17 × 8 cm encapsulated mass was found on the right lower chest cavity arising from the mediastinal pleura with a long vascularized pedicle. The tumour was compressing and displacing the right lower lobe of the lung without apparent infiltration of it (Fig. 2). Complete excision of the tumour was achieved as well as a wedge of the right lower lobe of the lung in contact with the tumour which appeared macroscopically compressed. No continuity with the thymic gland was observed.
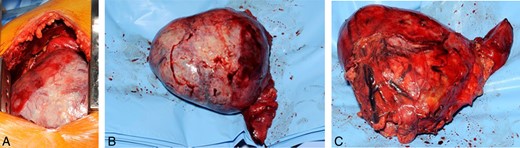
(A) Macroscopic view of the tumour through right anterolateral thoracotomy (surgeon's view from the anterior aspect of the patient); (B) lateral view of the tumour, showing surfaces in contact with chest wall and diaphragm; and (C) medial view of the tumour, notice pedicle clipped.
The pathology report confirmed a tumour composed of chords of epithelioid cells mixed with small cells, positive on immunohistochemistry for AE1/AE3, bcl-2, MOC31 and BerEP4. Although negative for CEA and EMA, the appearances favour a diagnosis of a type B2 thymoma. No evidence of invasion was assessable, and the lesion appeared completely excised. The lung tissue was reported as alveolated lung with focal pleural inflammation but no evidence of malignancy.
The post-operative course was uneventful. In the follow-up post-surgery, the patient remains asymptomatic.
DISCUSSION
The differential diagnoses for an intrapleural tumour are solitary fibrous tumour, malignant mesothelioma, sarcomas and secondary malignancies [3–5]. The histopathology and immunohistochemistry analysis are highly valuable for diagnosis.
Like the normally located thymomas, these tumours show a variable evolution from an indolent non-invasive form to an infiltrative and metastatic one. The Masaoka classification, based on the invasion of the capsule of the tumour and adjacent structures or distant metastases and the WHO classification, based on histological features, are both considered independent prognostic factors. Other important factors related to the outcome are the completeness of resection and the diameter of the tumour [1, 2].
Therefore, a complete surgical resection is the key for a long-term better prognosis. For completely resected thymomas, the administration of adjuvant treatment does not increase the survival, which is 80% at 10 years. Despite that, local recurrences have been occasionally reported, and a long-term follow-up is strongly recommended [1, 2].
CONFLICT OF INTEREST STATEMENT
None declared.



