-
PDF
- Split View
-
Views
-
Cite
Cite
Nicholas Birkett, Ibraheim El-Daly, Hajir Ibraheim, Chima Mbubaegbu, Metallosis following full thickness wear in total hip arthroplasty, Journal of Surgical Case Reports, Volume 2015, Issue 9, September 2015, rjv122, https://doi.org/10.1093/jscr/rjv122
Close - Share Icon Share
Abstract
Extreme wear through the metal-backed acetabular cup following total hip arthroplasty is rare, as symptoms such as pain and disability will usually manifest earlier. We present the second reported case of extreme wear in a 78-year-old male patient, who presented 20 years following an uncemented total hip replacement with a 3-year history of hip pain, clicking on ambulation and worsening mobility. Radiographs demonstrated that the femoral head had migrated superolaterally through the polyethylene liner and the acetabular cup, and was articulating with the superior wall of the acetabulum causing bony destruction. Metallic fragments were also evident. A review of the current literature on metallosis suggests that should there be any clinical suspicion, blood metal ion levels are monitored and an MARS-MRI scan performed if indicated. If metallosis is detected, then revision surgery can be attempted at an earlier date, where the procedure is not as technically difficult.
INTRODUCTION
Wear following total hip replacement (THR) is well documented and often leads to revision surgery, which can be complex and demanding. Revision rates are reported to be 2–6% at 10 years, depending on the prosthesis used. The majority are due to aseptic loosening [1].
Symptoms typically manifest following significant acetabular wear, at which point revision is usually considered. If the wear leads to metal-on-metal articulation, metallosis may result with its associated complications [2].
Metallosis is defined as the deposition of metal debris within periprosthetic soft tissue and bone. This can cause chronic inflammation, accelerated wear, prosthetic loosening and in advanced cases osteolysis. This complication is typically seen in ∼5% of metal on metal implants [3].
We present the second reported case of extreme wear through the metal-backed acetabular cup causing metallosis.
CASE REPORT
A 78-year-old gentleman with an uncemented left THR performed 20 years earlier for osteoarthritis was reviewed in clinic. He was referred with increasing left hip pain, clicking on ambulation and worsening mobility over 3 years, having now become wheelchair dependent. His past medical history included early dementia, type 2 diabetes and hypertension.
Examination of the left hip revealed a fixed flexion deformity of 30° with a shortened wasted left leg of 2.5 cm. Hip movements were grossly reduced and exquisitely painful. The scar was well healed with no sinuses, normal skin temperature and no overlying skin changes or palpable soft tissue masses.
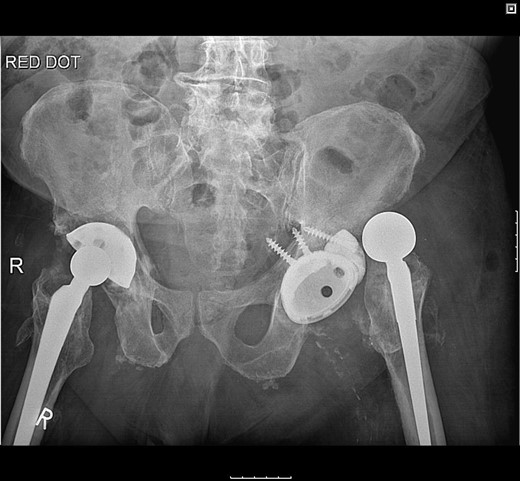
Pelvic radiographs demonstrated that the femoral head had migrated superolaterally through the polyethylene (PE) liner and the acetabular cup with metallic fragments inferior to this, and was articulating with the superior wall of the acetabulum causing bony destruction. There was no radiographic evidence of loosening to the stem (Fig. 1).

Pelvic radiograph demonstrating superolateral migration of the femoral head, metallic fragments around the neck and bony destruction of the acetabular wall.
The patient was subsequently scheduled for revision surgery of the acetabular component. Intraoperatively, there was blackening of the periprosthetic tissue and metal debris throughout. The PE liner remained engaged within the acetabular cup with significant wear through its back. The femoral head had migrated superolaterally through the acetabular cup and was articulating with the superior acetabular wall causing bony destruction. The acetabular cup remained well fixed within the acetabulum with good bony ingrowth (Figs 2 and 3).

The acetabular component showing extreme wear-through and metallic fragments.

The femoral stem was kept firm in its proper position. Structural porous titanium acetabular augment (Regenerex™), reinforced with a cancellous allogeneic bone graft, was used to reconstruct the superior acetabular wall. The cup was completely revised using a Biomet® Regenerex Ringloc® multihole 56-mm acetabular cup and a Hi-wall Ringloc-x PE 54-mm liner. The previous 32-mm femoral head was replaced with a Bioball® 36-mm metal head and a Bioball® adapter standard (0 mm) Taper 11/13 (4° 3°), correcting the offset and achieving stability (Fig. 4).

A post-revision radiograph demonstrating a structural graft using the acetabular augment (Regenerex™) and revised cup in situ.
Postoperatively, the patient fell on the ward resulting in posterior dislocation (Fig. 5) requiring an open reduction. Subsequently, the patient developed a superficial surgical site infection, which resolved with antibiotic therapy. Three months following discharge, the patient was pain-free and could ambulate with a Zimmer frame.
Radiograph following postoperative fall demonstrating posterior dislocation.
DISCUSSION
Wear-through the PE liner and metal acetabular component is extremely rare. To our knowledge, there is only one other reported case of metallosis following such extreme wear [4]. Causes of PE wear in THR are multifactorial. The patient's level of activity is the main factor affecting outcome, with prostheses inserted in younger, more active patients being associated with reduced longevity [2].
Metallosis can lead to implant failure or a foreign body reaction. Small metal particles can increase wear rates by interfering with smooth articulation, instigating an inflammatory response within the joint [5].
When considering revision in metallosis, the following risk factors should be taken into account: (i) whether the patient is symptomatic, (ii) the size and shape of the particular prosthesis and (iii) if there is evidence of extreme wear or metallosis on plain radiographs.
Characteristic features of metallosis on plain radiographs include eccentric alignment of the femoral head, suggesting extreme wear and radiolucency around the joint (the bubble sign), suggesting deposited metallic debris [6]. However, plain radiographs alone have been shown to have poor sensitivity, with signs absent in over half the cases [7]. Computed tomography imaging can be useful in evaluating metallosis. Characteristic findings include high-density material outlining the joint capsule or bursa [8].
The imaging modality of choice is metal artefact reduction sequence of magnetic resonance imaging (MARS-MRI). It has been shown to reliably diagnose and confirm the extent of metallosis, identifying any pseudotumours following metal-on-metal hip replacements [9].
Metal ion levels are another indicator for detecting early metallosis following arthroplasty. A review of the current literature suggests that a threshold >4.5 ppb of cobalt/chromium should trigger further investigation with MARS-MRI [10].
It is necessary for patients to have regular clinical and radiological follow-up after a total hip arthroplasty. When a severely worn acetabular shell is recognized, revision surgery should be performed early. If the damage to the metal shell is minimal, then it is acceptable to simply replace the liner. In the case of extreme metallic wear, then a more comprehensive revision is required.
Extreme wear and associated metallosis of this kind are rare. The fact that our patient remained relatively asymptomatic until the wear was very severe highlights the importance of regular radiographs and follow-up. Clinical suspicion of metallosis should lead to monitoring of blood metal ion levels, and an MARS-MRI scan if indicated. If metallosis is detected, then revision surgery can be attempted at an earlier date, where the procedure is not as technically difficult.
CONFLICT OF INTEREST STATEMENT
None declared.



