-
PDF
- Split View
-
Views
-
Cite
Cite
Harufumi Maki, Masaki Azuma, Hitoshi Kanamaru, Motohiro Nishiyama, Kazuya Okamoto, Takahiro Shimamura, Kennoki Kyo, Atsushi Maema, Toshio Nakamura, Motoaki Shirakawa, Hidetaro Yokoyama, Transabdominal approach assisted by thoracoscopic drainage for lower esophageal perforation, Journal of Surgical Case Reports, Volume 2015, Issue 12, December 2015, rjv151, https://doi.org/10.1093/jscr/rjv151
Close - Share Icon Share
Abstract
The effectiveness of use of thoracoscopy for esophageal perforation has not been fully evaluated. We herein report a case of esophageal perforation for which a transabdominal approach assisted by thoracoscopic drainage was performed.
INTRODUCTION
Esophageal perforation, first reported by Boerhaave in 1724, is still a life-threatening disease associated with a high mortality rate of 20–40% [1]. This dismal prognosis may be related to contamination of the mediastinum or pleural cavity, requiring thoracotomy and extensive surgical intervention [2]. Introduction of thoracoscopy instead of thoracotomy in the treatment of esophageal perforation might be not only helpful for irrigation and drainage but also reduce the respiratory compromise in critically ill patients, thereby improving the surgical results. We herein report a case of esophageal perforation for which the supplementary use of thoracoscopy was favorable in exploring the thoracic cavity and providing appropriate drainage.
CASE REPORT
A 67-year-old man presented with vomiting and epigastric pain. He had a history of duodenal ulceration and emergent laparotomies for repeated duodenal perforation, resulting in stenosis of the second portion of the duodenum. The patient was referred to our hospital for evaluation of vomiting. He exhibited upper abdominal guarding on physical examination. His blood chemistry revealed no abnormal findings with the exception of a mild increase in the C-reactive protein level (2.1 mg/dl). His nutritional state was maintained. Dynamic computed tomography revealed massive right pleural effusion with pneumomediastinum. A defect was present in the lower esophagus, his stomach was dilated and the proximal duodenal wall was thickened (Fig. 1a and b). Thoracoscopic exploration was performed prior to laparotomy in the left semi-lateral decubitus position with 2 ports under differential lung ventilation. The right pleural cavity was severely contaminated with brownish pleural effusion and was thus irrigated under thoracoscopy, but the perforated site was not identified. Laparotomy was then performed, which revealed a 4-cm longitudinal defect on the right side of the lower esophagus via esophageal hiatus (Fig. 2). The defect was closed by direct suturing with 4-0 pieces of monofilament strings and reinforced by using the greater omentum. The surgical field was irrigated, and a feeding jejunostomy was created. A 19F blake drain (Ethicon, Inc., Sommerville, NJ, USA) was placed in the lower mediastinal space via abdominal cavity, and a 20F thoracic drain (Sumitomo Bakelite Co., Ltd, Tokyo, Japan) was placed in the right thoracic cavity via the port site. The position of the mediastinal drain was cranially adjusted using the thoracoscopy (Fig. 3a and b). Extubation and enteral feeding via the jejunostomy tube were initiated on Day 2. Endoscopic dilatation was performed due to esophageal stenosis. The patient was discharged on Day 60 without mediastinitis, pneumonia or empyema.
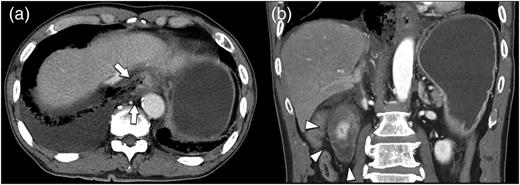
Chest and abdominal computed tomography findings. (a) Horizontal cross section. The right wall of the abdominal esophagus is perforated (arrows). (b) Coronal section. The duodenal wall is markedly thickened (arrowheads).
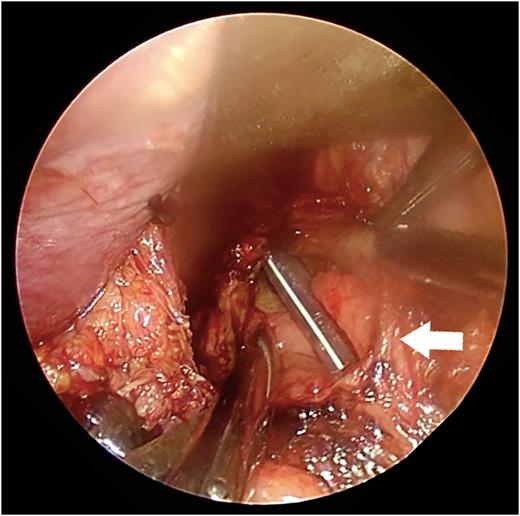
A picture of the perforated site. A nasogastric tube was found via the perforated site during transabdominal manipulation (arrow).
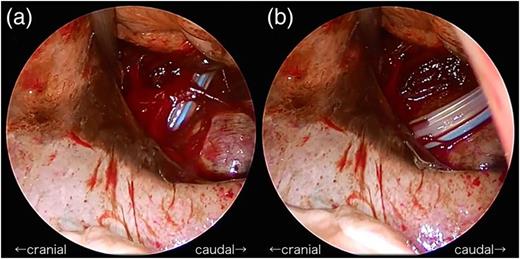
Thoracoscopic mediastinal drainage. (a) The angle of the drain was too steep at first. (b) The drain was successfully inserted in the deepest region of the chest by adjusting the angle of the drain.
DISCUSSION
Esophageal rupture can cause shock and dyspnea due to the progression of mediastinal emphysema or pneumothorax. Vomiting is the most common trigger of spontaneous esophageal rupture; however, duodenal stenosis secondary to previous benign ulceration as a cause of vomiting leading to esophageal perforation is rare. Tanaka et al. reported the fourth case of esophageal perforation related to pyloric stenosis caused by duodenal ulcer [3]. Three of the four patients underwent emergent operation using transabdominal approach via the esophageal hiatus. Our case was unique in that he had undergone transabdominal approach combined with thoracoscopic approach.
The usefulness of the thoracoscopic approach for esophageal perforation has not been fully evaluated, and the consensus on this surgical procedure has not been established. To our knowledge, 40 cases in 19 articles written in English have been reported so far who underwent thoracoscopic approaches to esophageal perforations, since Hutter et al. firstly reported irrigation combined with thoracoscopy for the management of esophageal perforation in 1985 and thoracoscopically assisted direct suturing of an perforation site was first reported by Kiel et al. in 1993 [4, 5]. Thoracoscopic suturing was performed in 16 of the 40 cases, thoracoscopic drainage in 12 and thoracoscopic T-tube placement in 2. Added surgical procedures such as feeding jejunostomy were conducted in 15 of the 40 cases, which implies diversity of treatment of this disease. In 2011, Haveman et al. reported a historical cohort study comparing video-assisted thoracoscopic surgery with open thoracotomy [2]. They stated that video-assisted thoracoscopic surgery was as safe as the open approach, and the overall in-hospital mortality was 8% in each group. The study showed that adequate surgical drainage of the mediastinum and pleural cavity should be the keys in the treatment of esophageal perforation because the most common cause of death was multiorgan failure secondary to sepsis. On the other hand, thoracoscopic surgery should be avoided when the vital signs of the patient are unstable. Thoracotomy or laparotomy should be added to reduce postoperative complications and achieve infection control [6].
In the present case, esophageal perforation was diagnosed based on the patient's medical history, symptoms and computed tomography findings, allowing for treatment to begin 8 h after the initial episode of vomiting. Emergent surgery is necessary in cases of perforation into the pleural cavity and resultant severe contamination. The esophageal defect can be primarily sutured if it is detected within 24 h after rupture. Yamashita et al. reported successful treatment of spontaneous esophageal rupture with an omentum flap to reinforce the suture line [7]. The authors recommended enteral nutrition from the jejunostomy site because fasting was required. Meanwhile, Sakamoto et al. emphasized the usefulness of T-tube drainage for the late management of esophageal perforation [8]. In the present case, surgical treatment was started within 8 h after rupture, which may have resulted in the favorable outcome after primary closure of the perforated site, except for remaining esophageal stenosis.
CONFLICT OF INTEREST STATEMENT
None declared.
ACKNOWLEDGEMENTS
The authors are grateful to Yoshihiro Sakamoto, MD, for his advice and assistance in the preparation of the manuscript.



