-
PDF
- Split View
-
Views
-
Cite
Cite
Selam Yekta Sendul, Cemile Ucgul, Burcu Dirim, Mehmet Demir, Zeynep Acar, Dilek Guven, A difficult surgical approach for primary orbital hydatid cyst: transconjunctival medial orbitotomy, Journal of Surgical Case Reports, Volume 2015, Issue 12, December 2015, rjv150, https://doi.org/10.1093/jscr/rjv150
Close - Share Icon Share
Abstract
Hydatid cysts rarely appear isolated in the orbital cavity without involvement of other organs. The cysts are usually located in the retrobulbar region, and may be extraconal or intraconal. Herein we present a case of primary orbital cyst hydatid that is adjacent to the medial rectus muscle and optic nerve in the intraconal space and the difficulties during the surgical and medical treatment period.
INTRODUCTION
Hydatid cyst is a parasitic disease mostly caused by larval stage of Ecinococcus granulosus. Orbital hydatidosis is rare, accounting for only 1% of all hydatid cysts [1].
CASE REPORT
A 24-year-old female patient was admitted to our clinic with low vision and proptosis of her right eye for a year. Visual acuity was reduced to finger counting at a 2-feet distance with an accurate projection of light. Ocular movements were restricted in all directions. Ophthalmic examination revealed the manifest proptosis of her right eye and measured 22 mm by Hertel's exophthalmometer. Anterior segment examinations of her both eyes were unremarkable. Fundus examination revealed macular edema, like the wrinkles in the macular region, papilledema with tortuosity of blood vessels on her right eye (Fig. 1a and b).
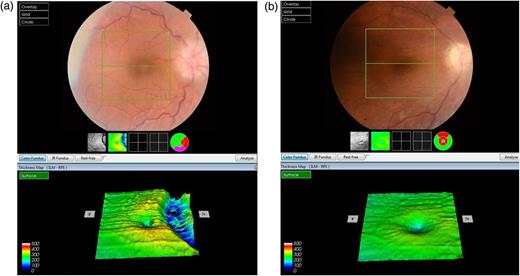
(a) Preoperative OCT and fundus photography of the right eye show the papilledema and macular pucker. (b) After first operation, control OCT and fundus photography in the second postoperative month show that both papilledema and macular edema subside remarkably.
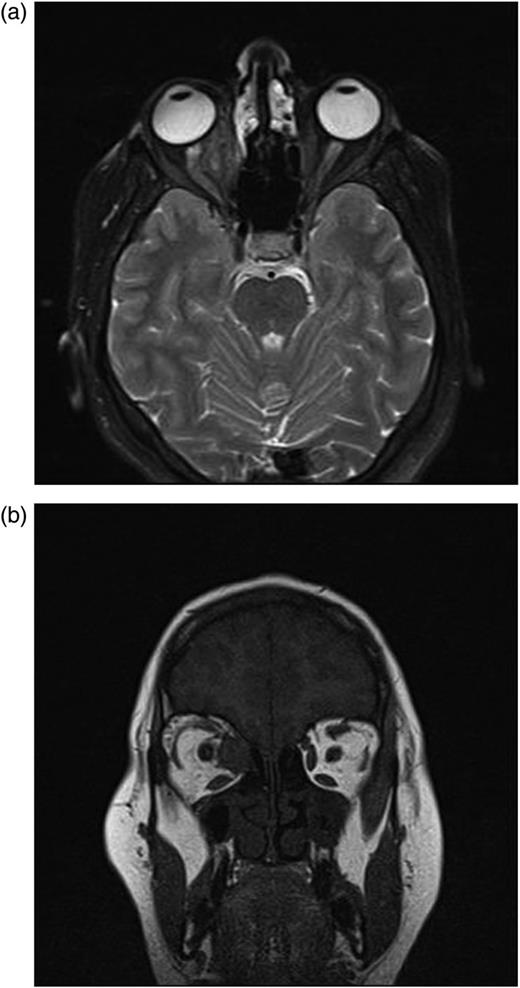
A complete blood cell count and serum laboratory values were normal without mild eosinophilia. Axial-coronal orbital magnetic resonance imaging (MRI) revealed a well-defined homogenous unilocular lesion in intraconal region of the right orbita which was hypointense on T1-weighted images and hyperintense on T2-weighted images after an intravenous injection of gadolinium-ethoxybenzyl-diethylenetriamine pentaacetic acid (Fig. 2a and b). The lesion was adjacent to optic nerve and medial rectus muscle and exerting pressure on the optic nerve and displacing optic nerve laterally. Approximate dimension of the lesion was 2 cm × 2 cm × 2 cm (Fig. 2a and b). Because it was difficult to distinguish hydatid cyst from other mass lesions of the orbita via MR, other mass lesions like neurocysticercosis, dermoid, lipodermoid, mucocele, encephalocele, inclusion cyst, teratoma, hematocele, schwannoma and paraganglioma were considered in the differential diagnosis of hydatid cyst.
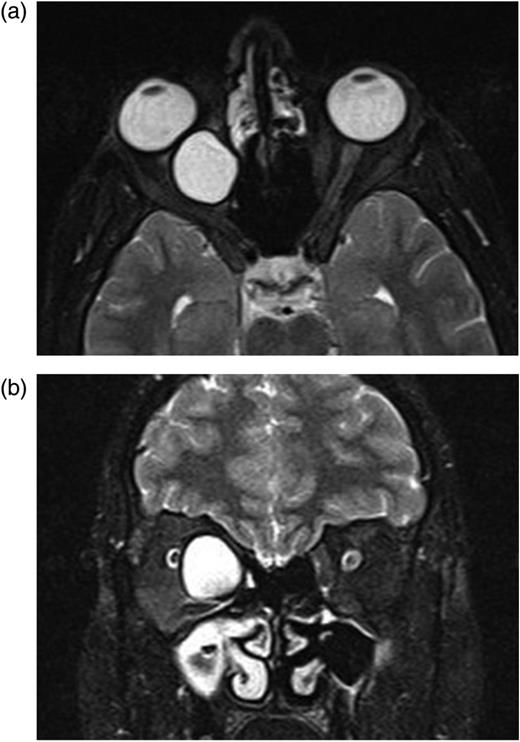
(a and b) Axial-coronal orbital magnetic resonance imaging show the homogenous unilocular lesion that is adjacent to optic nerve and medial rectus muscle in the intraconal space and displacing optic nerve laterally.
The patient underwent surgery via a medial transconjonctival orbitotomy approach. After medial conjunctival peritomy, we managed to reach intraconal space by separating medial rectus muscle from insertion area. We reached the solid, veinless mass via dissection from around area in difficulty. Intraoperatively the outer capsule of the exposed cyst was identified and an effort was made to dissect it from retrobulbar tissues by using hypertonic saline-soaked cotton patties. It was almost impossible for us to remove the cyst without rupture due to the anatomic disadvantage of the surgery area. Because of this, we ruptured the cyst wall consciously. To prevent the spread of the parasitic disease, washing with %0.9 hypertonic saline solution and continuous aspiration were applied simultaneously. The whole membrane of the cyst was removed totally (Fig. 3a and b). At the end of the surgery, medial rectus muscle was sutured to insertion area. The excised sample was set for histopathological examination of the excised sample confirmed the diagnosis of hydatid cyst (Fig. 3c).
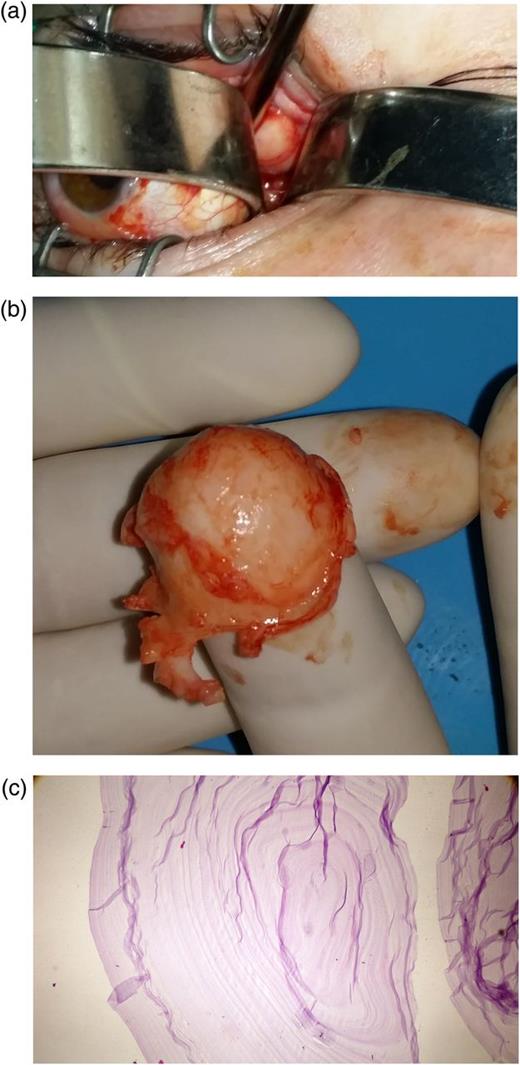
(a) The appearance of the peroperative solid mass that locates intraconal space. (b) The appearance of the cyst capsule that is thick, whitish and fragile. (c) Histopathologic appearance of the hydatid cyst staining Haematoxylin and Eosin (H&E).
On the first postoperative day, due to the severe chemosis and reaction of anterior segment, 1000 mg prednisolone was applied intravenously for 3 days and then was maintained at 1 mg/kg/day orally. Systemic albendazole 400 mg was applied twice a day for 2 months.
On the third postoperative day, her ocular motilities were not restricted. Visual acuity recovered to 1/10 on Snellen chard. The papilledema disappeared with remaining disc pallor. The macular edema subsided remarkably.
In the second postoperative month, the findings of ocular examination were the same. Control MRI revealed that there was a new small cyst in the intraconal space (Fig. 4a and b). Based on these findings, we planned the second operation via again medial transconjunctival orbitotomy. Peroperatively, we could not find remarkable cyst capsule. To prevent any inoculation, surgery area was washed with %0.9 hypertonic saline solution. Due to the postoperative edema, 80 mg systemic prednisolone was applied for 3 days. Systemic albendazole was applied twice a day for 2 months.
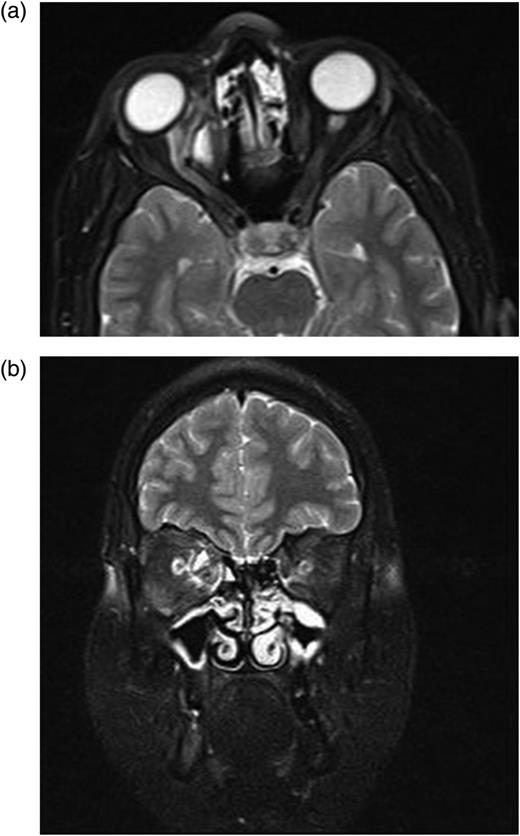
(a and b) After first operation, control MRI in the second postoperative month shows a small cyst displacing optic nerve laterally.
After second operation, in the first postoperative month, her ocular motilities were not restricted. Visual acuity was maintained at the same level (1/10). Control MR revealed no cystic structure except granulation tissue (Fig. 5a and b).
(a and b) After second operation, Control MRI in the first postoperative month shows granulation tissue.
During the follow-up, the patient was planned to set albendazole treatment for 1 week each month for 3 months.
This case was considered as a primary infection, because there was no previous history of hydatid disease and no findings of liver and lung cysts on radiological examination. The study was conducted in accordance with the tenets of the Declaration of Helsinki by obtaining written consent from patient, with the approval of the local ethical review board.
DISCUSSION
Hydatid is a disease transmitted through the foods infected with the eggs of the parasite or direct contact with infected dog feces. The larva can be placed in many organs like the liver, lung, heart, bone and brain. Hydatid cysts are most commonly located in the liver (60–70%) and the lungs (20%). The orbita is a very rare location for echinococcal infestation and makes up less than 1% of all cystic involvements [2–4]. Altınörs et al. surveyed the literature on central nervous system hydatidosis in Turkey and found that 22 of 336 cases were located in the intraorbital space [1].
Although orbital hydatid cysts usually spread from another area of the body via the portal and systemic circulation and then they are named as secondary orbital hydatid cyst, primarily orbital hydatid cysts that are solely located in the orbita are rarely seen [5]. Primary orbital hydatid cysts may be located in intraconal or extraconal space. The hydatid cyst of our patient was located in intraconal space between the medial rectus muscle and the optic nerve.
Although there are reports in the literature of multiple intraorbital hydatid cyst, orbital hydatid cysts are solitary lesions in the majorty of the cases [6] as our case had solitary lesion.
The most commonly seen clinical symptoms and signs of the orbital ecinococcosis are nontender, nonpulsatile proptosis, visual deterioration, diplopia, the restriction of ocular motolities, chemosis, eye lid edema, conjunctivitis, papilledema, macular edema, even retinal detachment. Most of them are due to the compressive effect of the cyst. The most important compressive effects are the compressive optic neuropathy and optic atrophy [7, 8]. Hydatid cysts grow an average of 1.5 cm each year. Due to the limited space in the orbital cavity, patients usually become symptomatic before 2 years [9, 10]. In our case, the most important complaints were proptosis and visual deterioration for a year.
The diagnostic work-up of orbital hydatid cyst includes serological tests, orbital ultrasound, computerize tomograpy (CT) and MRI. Many serological tests can be used in diagnosis of Echinococcosis, but in orbital hydatidosis they usually give negative results. The Cassoni's intradermal (ID) test, counter immune-electrophoresis, double diffusion test and indirect hemagglutination test have been used. The sensitivity of these tests in orbit is lower than other organs due to the less exposure of the parasitic proteins to the immune system. Because of these, the most important diagnostic method of the hydatid cyst is imaging methods like CT and MRI [7].
The most important treatment of hydatid cyst is the surgery that can manage without rupture. Whereas, due to small size and complexity of the orbital anatomical region, the rupture and spreading to the other parts are sometimes inevitable. Because of these, sometimes, the surgeon needs to rupture of cyst consciously. We tried to remove the cyst via medial transconjonctival orbitotomy method and it was not possible that we removed the cyst without rupture that was between optic nerve and medial rectus muscle in intraconal space. Because of this, we ruptured the cyst and to prevent the spread of the parasitic disease, washing with %0.9 hypertonic saline solution and continuous aspiration were applied simultaneously. Most probably, due to the inoculation we needed a second operation. Although we saw the surgery area as clean in the second operation, the patient's best corrected visual acuity was only 1/10. The presence of the cyst about for a year and compressive effect of the cyst to the optic nerve may be causes of this low vision. Because hydatid cysts are a disease of young patients and are usually progressive and delayed treatment may lead to blindness by optic nerve compression [5].
Consequently, we should always include the diagnosis of hydatid cyst at differential diagnosis of unilaterally, slowly progressive proptosis.
CONFLICT OF INTEREST STATEMENT
None declared.



