-
PDF
- Split View
-
Views
-
Cite
Cite
Andrew Senior, James Andrew Douglas, Stuart Thompson, Unilateral vocal cord palsy and dysphagia: an unusual presentation of cerebellopontine angle meningioma, Journal of Surgical Case Reports, Volume 2015, Issue 10, October 2015, rjv129, https://doi.org/10.1093/jscr/rjv129
Close - Share Icon Share
Abstract
Cerebellopontine angle (CPA) tumours are the most common neoplasms in the posterior fossa, accounting for 5–10% of intracranial tumours. Most CPA tumours are benign, with most being vestibular schwannomas. Meningiomas arising from the jugular foramen are among the rarest of all with very few being described in the literature. Treatment options vary considerably as experience with these tumours is limited. One option is a skull base approach, but this depends on size, location and ability to preserve lower cranial nerve function. This can be extremely challenging and is accompanied by high mortality risk; therefore, a more conservative option must be considered. This case report highlights the difficulty in management of patients with jugular fossa meningiomas, including appropriate investigations, analysis of surgical versus conservative treatment and associated complications. Furthermore, we elaborate the decision-making process pertaining to the tailoring of the surgical route used for the resection of jugular foramen meningiomas. (Jugular Foramen Meningioma, cerebellopontine angle).
INTRODUCTION
Cerebellopontine angle (CPA) tumours are the most common neoplasms in the posterior fossa, accounting for 5–10% of intracranial tumours. Most CPA tumours are benign, with most being vestibular schwannomas (VS) and meningioma [1].
Meningiomas arising from the jugular foramen are among the rarest of all with very few being described in the literature. Symptoms and signs are dependent on relationship to lower cranial nerves and jugular bulb but like VS, unilateral hearing loss (95%), tinnitus (80%), vertigo (75%) and headache (25%) are common presenting features.
Treatment options vary considerably as experience with these tumours is limited. One option is skull base approach and surgical debulking, but this depends on size, location and ability to preserve lower cranial nerve function, in particular nerves IX and X [2]. Surgical indications vary between units due to the limited exposure to management of this pathology.
We describe a rare case of hoarse voice and dysphagia in a patient who was found to have a large jugular foramen meningioma.
The purpose of this case report was to evaluate the management of patients with jugular fossa meningiomas, including appropriate investigations, analysis of surgical versus conservative treatment and associated complications. Furthermore, we elaborate the decision-making process pertaining to the tailoring of the surgical route used for the resection of jugular foramen meningiomas.
CASE REPORT
A 78-year-old non-smoking, teetotal female presented to voice clinic with a 6-month history of progressive dysphonia and dysphagia. Focussed history revealed a progressive left-sided hearing loss. Otoscopic examination was normal; however, a pure tone audiogram confirmed a dead left ear. Flexible nasoendoscopy (FNE) revealed unilateral left vocal cord palsy with significant pooling of saliva.
Urgent skull base to diaphragm computed tomography (CT) scans (Fig. 1) suggested a large (4 × 3.5 cm) mass within the left posterior fossa and no lung lesions. There were no changes to the pre-existing renal cysts.
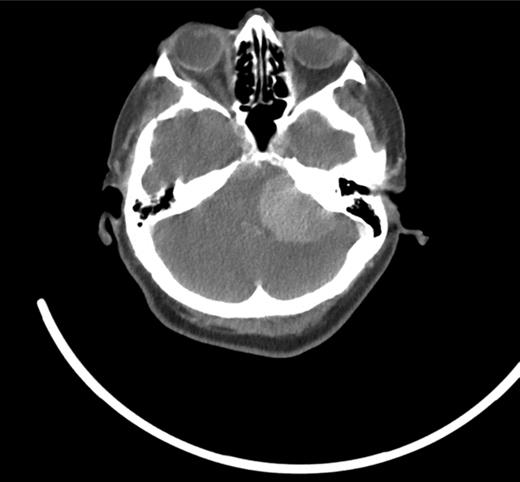
CT scan—large (4 × 3.5 cm) mass within the left posterior fossa.
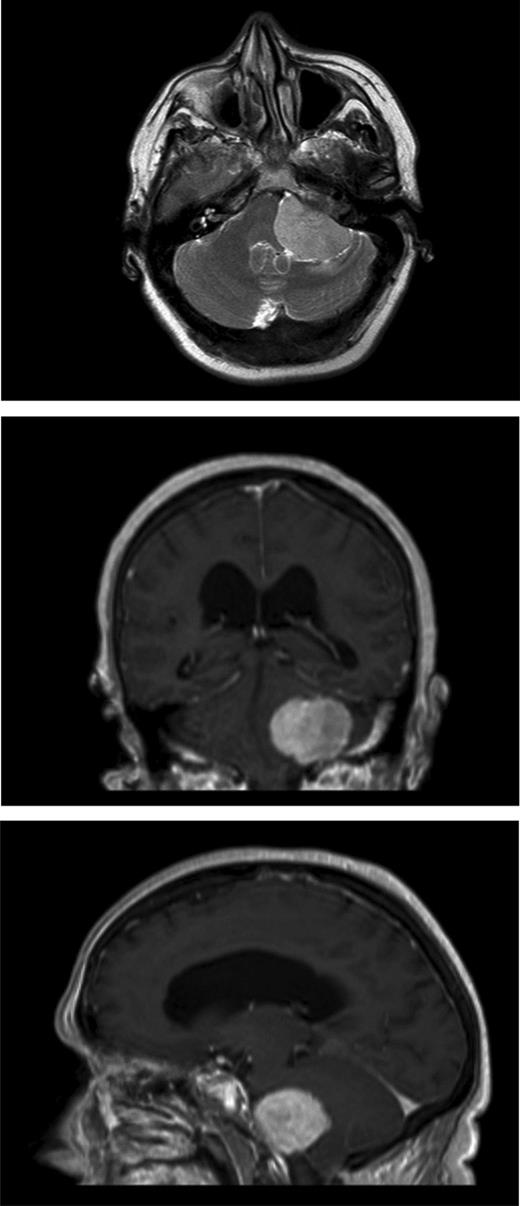
Magnetic resonance imaging (MRI) head confirmed the presence of a primary posterior cranial fossa meningioma that was surrounding the jugular foramen, compressing the brainstem and vagus nerve (Fig. 2).
Feeding was commenced by insertion of a percutaneous endoscopic gastrostomy (PEG), and symptoms of increased intracranial pressure (ICP) were managed medically with high-dose steroids and anti-emetics.
Neurosurgical multidisciplinary team (MDT) discussion felt that the patients' morbidity and mortality risk was too great to warrant surgical intervention and that gastrostomy feeding should continue due to the high risk of aspiration. Second opinion from a tertiary neurosurgical unit felt that a ventriculoperitoneal (VP) shunt would be necessary if the patient developed any signs of increased ICP in the future. Subsequently, the patient was discharged home and managed conservatively.
DISCUSSION
Primary jugular foramen meningiomas arise from arachnoid cells that line the jugular bulb in the jugular fossa. In many of the reported cases, jugular foramen meningiomas mimicked glomus jugulare tumours and lower cranial nerve neuromas. They have an intimate relationship with the lower cranial nerves, the jugular bulb and vein, and the temporal bone.
Lesions that originate in the jugular foramen or the area of the hypotympanum may be associated with pulsatile tinnitus, hearing loss, aural fullness and dysphagia; less common signs and symptoms result from invasion of cranial nerves IX–XII and include hoarseness, vertigo and balance dysfunction. It seems, therefore, prudent that any ear, nose, throat surgeon should consider an intracranial tumour as a diagnosis when presented with a patient with vocal cord paralysis.
Primary jugular foramen meningioma is a common tumour in an unusual location. Furthermore, differentiation of primary jugular foramen meningioma from the more common masses, specifically paraganglioma and schwannoma, has important prognostic and therapeutic implications, which increases the importance of preoperative diagnosis.
Clinical decision-making, therefore, is highly dependent on appropriate investigations. Pre-MDT radiology should be tailored to define local anatomy of the local vasculature, jugular foramen, fossa, temporal bone and condyles. This should, therefore, include CT scanning, MRI with and without contrast, and MR angiography.
Otolaryngological assessment must include fundoscopy to rule out cholesteotoma and pure tone audiogram to assess the presence of a dead ear.
This case highlights the need for two key investigations. FNE should be undertaken to evaluate vocal cord paralysis. The speech and language team also need to assess the patient's ability to swallow, as this will dictate the need for feeding aids pre- and post-op.
Multiple lower cranial nerve deficits are common sequelae of surgical resection of jugular foramen lesions. Meningioma patients tend to have greater cranial nerve paralysis than other tumours ∼60% compared with 30% for glomus jugulare and 15% for schwannomas.
They are often adherent to the nerves within the confines of the jugular foramen, which in some cases makes it impossible to perform a total tumour resection with preservation of neural integrity; in such cases, a subtotal resection may be a better option, possibly followed by stereotactic radiosurgery (SRS) [3].
Sanna et al. [4] retrospectively assessed 13 cases. They concluded that surgical resection remains the treatment of choice for jugular foramen meningiomas and is possible with a variety of microsurgical techniques. However, they also reported high complication and recurrence rates, 15 and 7.7%, respectively. Death was secondary to aspiration pneumonia in two cases.
The surgical mortality risk remains high and is associated with postoperative cranial nerve palsy. Therefore, preoperative dysphagia/nerve palsy, invasion of local neurovascular structures and premorbid state should be considered as reasons for conservative management.
If conservative management is chosen, this focusses on symptom/risk control including PEG feeding to reduce the risk of aspiration and steroid/VP shunt use to improve medical symptoms of headache and sickness. The patient may also require tracheostomy and/or vocal cord medialization if aspiration risk is high or airway protection is of concern.
Nevertheless, all patients must be discussed with neurosurgical MDT urgently as with careful, extensive preoperative evaluation, planning and appropriate tailoring of surgical approach, radical tumour resection can be achieved with the expectation of a good clinical outcome.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- brain tumors
- deglutition disorders
- posterior fossa of cranial cavity
- cerebellopontine angle
- decision making
- drug administration routes
- meningioma
- acoustic neuroma
- base of skull
- surgical procedures, operative
- vocal cord paralysis
- cranial nerves
- mortality
- neoplasms
- jugular foramen
- conservative treatment



