-
PDF
- Split View
-
Views
-
Cite
Cite
Elizabeth N. Kuhn, Akhil Muthigi, John Frino, Alexander K. Powers, The use of dual growing rods to correct spinal deformity secondary to a low-grade spinal cord astrocytoma, Journal of Surgical Case Reports, Volume 2015, Issue 10, October 2015, rjv128, https://doi.org/10.1093/jscr/rjv128
Close - Share Icon Share
Abstract
Pediatric intramedullary spinal cord astrocytomas are rare, and the majority are low grade, typically carrying a low risk of mortality, but a high risk of morbidity. Quality of life is, therefore, an important consideration in treating concomitant progressive kyphoscoliosis. Compared with fusion-based spinal stabilization, fusionless techniques may limit some complications related to early instrumentation of the developing spine. Another consideration is the timing of radiation therapy relative to both spinal maturity and spinal instrumentation. To date, there have been no reports of the use of a fusionless technique to treat spinal deformity secondary to an intramedullary spinal cord tumor. Herein, we report the use of fusionless spinal stabilization with dual growing rods in a boy with low-grade spinal cord astrocytoma after radiation therapy.
INTRODUCTION
Spinal cord low-grade astrocytomas have low mortality, but high morbidity, highlighting the need to prioritize functional outcomes. Multiple series report that severe progressive kyphoscoliosis in patients with intramedullary spinal cord tumors necessitates instrumented fusion in greater than one-third of the patients [1–3]. Treatment with laminectomy and/or radiation can lead to asymmetric vertebral growth further exacerbating kyphoscoliosis [4], often requiring surgical correction of spinal deformity [5].
Posterior fusion with instrumentation has been the standard of surgical treatment of scoliosis since its introduction. However, fusion-based techniques may adversely affect growth of the trunk and thoracic cavity relative to the extremities, impair pulmonary development and increase early mortality. A number of fusionless growth-sparing techniques have evolved for the treatment of early-onset scoliosis, though growing rod-type surgical techniques remain the most widely utilized.
Despite the availability of these techniques, fusionless surgery for the correction of spinal deformity secondary to a spinal cord tumor has not, to our knowledge, ever been reported.
CASE REPORT
A boy presented at the age of 4 years with leg length discrepancy, gait difficulty, significant right-sided rib hump and chest wall deformity and was found to have thoracolumbar dextroscoliosis with a 32-degree curvature (Fig. 2A). He had a Grade II functional status using the McCormick classification scheme [6]. Magnetic resonance imaging (MRI) demonstrated an intramedullary mass from T6 to T11 (Fig. 1). An open biopsy was performed at T8 with a limited laminotomy demonstrating low-grade astrocytoma.

Sagittal MRI T2-weighted demonstrating an intramedullary mass spanning T6 to T11. The mass measures 7.8 × 1.4 × 1.5 cm and is the largest in diameter at the T8 level where it demonstrates considerable cerebrospinal fluid effacement. There is no associated syrinx. Post gadolinium contrast imaging (not shown) shows patchy enhancement, most evident in the inferior aspect of the lesion.
Given the patient's excellent functional status, he was treated with vincristine and carboplatin using the protocol from CCG A9952 (Supplementary material, Appendix 1), though he was not enrolled in the trial. Our radiation oncology colleagues indicated that he would likely require radiation therapy should his tumor progress; however, radiation would be technically challenging if hardware was placed for scoliosis correction given hardware artifact and concerns for wound healing. It was thus recommended that surgical correction of his scoliosis be delayed as long as possible. Imaging throughout chemotherapy demonstrated stability of his curvature.
Twenty months after diagnosis, the patient was experiencing more frequent back and leg pain and continued to ambulate with a limp. Imaging demonstrated that the tumor was gradually enlarging over time. At that time, the patient began therapy with bevacizumab and irinotecan. After seven cycles of chemotherapy, therapy was stopped due to poor quality of life and poor tumor response.
Nearly 2 years after diagnosis, the patient's mother was concerned that his persistent back and leg pain resulted from his scoliosis. Ultimately, it was decided to proceed with radiation therapy, and the patient completed treatment of the thoracic spine to 50.4 Gy in 1.8 Gy fractions delivered via en face electrons.
One month after completing radiation (3 years since diagnosis), he reported increasing back pain along with failure to thrive and resultant difficulty attending school. Plain films demonstrated continued relative stability of his curvature at 44 degrees, and his increased back pain was attributed to early toxicity from radiation. Over the following 2 months, his back pain continued to progress, he also complained of neck pain and his mom noted subjective worsening of his curve. His narcotic requirement had increased, and imaging confirmed worsening of his thoracolumbar scoliosis with his curve measuring 64 degrees (Figs 2B and 3A). At this point, we recommended surgical intervention with placement of dual growth rods given the significant curve progression and deterioration in functional status (McCormick Grade III).
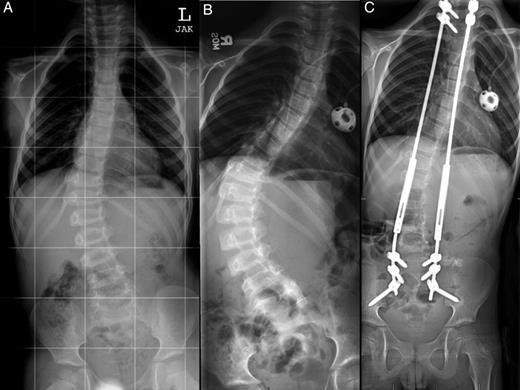
Anterior-posterior (AP) plain films of the spine at the time of diagnosis (A), after curve progression (B) and 1 year after growing rod insertion (C). Measured Cobb angles were 32 degrees (A), 64 degrees (B) and 22 degrees (C), respectively.

Clinical images prior to dual growing rod insertion (A) and 1 year after growing rod insertion (B).
We placed dual growth rods from T2 to the ilium with a posterior spinal fusion from T2 to T3 and L5 to the ilium. The surgical technique has been previously described in detail by Akbarnia et al. [7]. Motor evoked potentials and somatosensory evoked potentials remained stable throughout the entirety of the case. Postoperatively, he had full strength.
At his 1-month postoperative visit, the patient reported an interval decrease in his neck pain. However, 5 months after growing rod placement, the patient was seen in clinic for increased mid-thoracic back pain and subjectively increased prominence of his right thoracic muscle prominence. X-rays revealed a complete break in the right-sided rod at L3–4 with 5 mm of lateral displacement of the proximal fragment (Fig. 4). He subsequently underwent replacement of the fractured rod and lengthening of the entire construct.
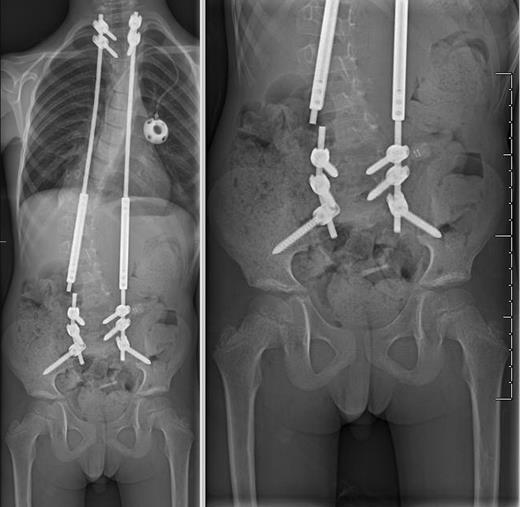
AP plain films demonstrating complete fracture of the right-sided growth rod with 5 mm of lateral displacement of the proximal fragment relative to the distal fragment.
He had three total lengthening procedures in the first 14 months since placement of the growing rods with improvement in his scoliotic curvature to 22 degrees (Figs 2C and 3B). Eighteen months after insertion of his growing rod construct, he developed hardware infection requiring hardware removal. He is scheduled to undergo definitive fusion in the near future. He has returned to his initial independent functional status with minimal gait abnormality (McCormick Grade II) and is able to participate in activities such as biking and skateboarding. He is now 10 years old.
DISCUSSION
The optimal treatment strategy for low-grade spinal cord astrocytomas is not clearly delineated with treatment options including surgery, chemotherapy and radiotherapy. Guss et al. recommend delaying radiotherapy until disease progression to spare the adverse effects of radiation on development, which are inversely related to age at treatment [8]. The patient presented here was treated with radiotherapy only after tumor progression, allowing radiotherapy to be delayed from 4 to 7 years of age. Thus, delaying radiation likely limited the effect of radiation on progression of this patient's scoliosis.
Dual growing rod techniques for spinal deformity correction have well-demonstrated safety and efficacy in the treatment of early-onset and congenital scoliosis [7]. Complication rates range from 15 to 58%, and the majority of complications can be easily corrected during planned lengthening procedures [9]. We are the first to report the use of any distraction-based surgical technique (in this case, dual growing rods) to correct a spinal deformity secondary to spinal cord tumor.
As growth-sparing surgical techniques for scoliosis continue to advance, we are likely to see them applied to a broader cohort of patients with spinal deformity as demonstrated in this case.
SUPPLEMENTARY MATERIAL
Supplementary material is available at the Journal of Surgical Case Reports online.
CONFLICT OF INTEREST STATEMENT
None declared.



