-
PDF
- Split View
-
Views
-
Cite
Cite
Vincent Nguyen, Hannah Vassaur, F. Paul Buckley, Spontaneous chylous ascites, chylomediastinum and bilateral chylothoraces encountered during laparoscopic incarcerated paraesophageal hernia repair, Journal of Surgical Case Reports, Volume 2015, Issue 10, October 2015, rjv124, https://doi.org/10.1093/jscr/rjv124
Close - Share Icon Share
Abstract
Chylous ascites is an accumulation of milky lipid-rich lymph in the peritoneal cavity. Spontaneous chyle leak is a rare occurrence, often associated with malignancy or cirrhosis. This is a report of spontaneous chylous ascites, chylomediastinum and chylothoraces encountered in the setting of an incarcerated paraesophageal hernia. A 60-year-old female presented to the emergency department with epigastric pain, dysphagia and vomiting. Clinical presentation and imaging were concerning for an incarcerated paraesophageal hernia, and the patient was taken to the operating room. During laparoscopic reduction of the hernia and repair, chyle was encountered in the peritoneal cavity, mediastinum and pleural spaces. Postoperatively, the chyle leak resolved with a nonfat diet. The unusual occurrence of a chyle leak in this case may have been due to compression of the thoracic duct within the chest by the incarcerated paraesophageal hernia.
INTRODUCTION
Chylous ascites is an accumulation of milky lipid-rich lymph in the peritoneal cavity caused by a disruption in the lymphatic system. It was first identified in 1694 by Richard Morton in a 2-year-old male who died with tuberculosis [1]. Chylous ascites is fairly rare in the clinical setting, with a reported incidence of approximately 1 in 20 000 presenting to the hospital [1–3]. Left untreated, it can lead to nutritional deficiency and in some cases immunosuppression [1]. In rare cases, patients presenting emergently with volvulus or appendicitis have incidentally been found to have chylous ascites upon surgical exploration [2–4]. Paraesophageal hernia can present acutely with gastric obstruction or strangulation at an estimated incidence of 1.2% per patient per year, the treatment for which involves laparoscopic or open hernia reduction, resection of the hernia sac, repair of the hiatal defect and fundoplication [5]. We report the unique observation of spontaneous chylous ascites, chylothoraces and chylomediastinum occurring in the setting of an incarcerated paraesophageal hernia.
CASE REPORT
A 60-year-old female with a long-standing gastroesophageal reflux disease and known type III paraesophageal hernia presented to the emergency department with acute epigastric pain, dysphagia and vomiting. She noted a 1-month history of progressive dysphagia as well. Computed tomography (CT) revealed a large paraesophageal hernia with significant surrounding fluid concerning for incarceration (Figs 1 and 2). Owing to these findings and her discomfort, emergent laparoscopic repair of her paraesophageal hernia was recommended.
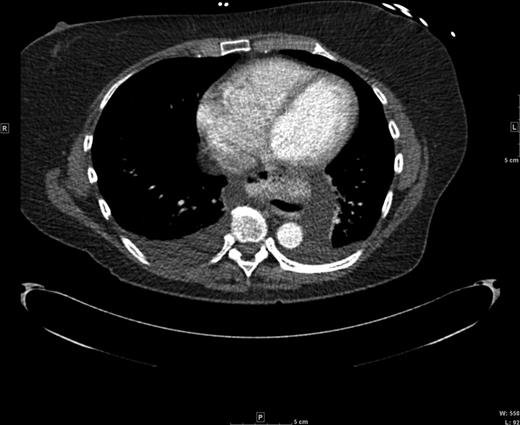
Axial CT view of the paraesophageal hernia and mediastinal fluid.
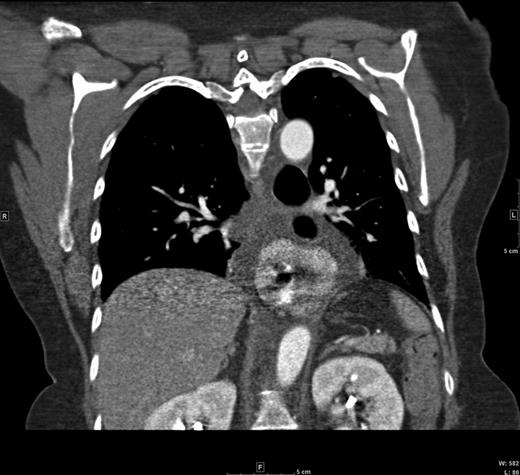
Coronal CT view of the paraesophageal hernia and mediastinal fluid.
Access to the peritoneal cavity began with a 2-cm incision at the umbilicus using the Hasson technique. After insufflation, four 5-mm trocars were introduced to the left and right upper quadrants. Chylous fluid was immediately visualized in the vicinity of the greater curvature of the stomach with the preponderance of the fluid at the splenic hilum and splenic flexure. Upon entering the lesser sac, chyle was found covering the pancreas as well. At this point, 20 mL of this chylous fluid was aspirated and sent for fluid analysis. The report later returned with triglyceride levels of 3362 mg/dl, consistent with chyle. During the hernia sac dissection, chylous fluid was visualized in the mediastinum and bilateral pleural spaces as well. No obvious source of leak was identified. Intraoperative EGD findings showed no sign of malignancy. The hiatal defect was primarily repaired and a posterior Toupet fundoplication was performed. Diagnostic laparoscopy and running the bowel revealed no abnormalities. Two 19-Fr Blake drains were placed: one in the lesser sac extending to the splenic flexure and one in the mediastinum. Trocar sites were closed in the usual fashion. Bilateral chest tubes, abdominal drain and mediastinal drain were placed to suction. Total operative time was 242 min.
Postoperatively, management began with placing the patient on a nonfat diet. Chest tubes drained about 100 mL of chylous fluid each, after which the output transitioned to serous. An abdominal and pelvic CT scan revealed no signs of malignancy that may have caused the chyle leak. Chest tubes and drains were removed by postoperative day 5. The patient was discharged on postoperative day 6 following resolution of chyle leak.
DISCUSSION
The etiologies for chylous ascites can be categorized as traumatic or atraumatic, with malignancy and cirrhosis comprising the majority of atraumatic causes in the developed world via disruption of lymphatic flow [1]. Spontaneous chylothoraces due to compression of the thoracic duct by a large substernal goiter and thoracic aorta aneurysm have been reported in the literature as well [6, 7]. Because the chyle leak resolved rapidly after reduction of the hiatal hernia in this case, it could be postulated that acute incarceration of the hernia within the chest led to significant inflammation and subsequent compression of the thoracic duct above the hiatus. The chyle found within the abdomen could be explained as a transudate from the chest, where the initial disruption to the lymphatic system likely occurred.
The most common presenting symptom for isolated chylous ascites is painless abdominal distention, but a subset of patients may present with peritoneal irritation or unspecified abdominal pain. Whether chylous ascites is suspected in a clinical setting or incidentally in the operative room, analyzing fluid to confirm diagnosis is critical. For this reason, abdominal paracentesis may be indicated when suspicion for ascites exists at the time of presentation. Chyle is classically defined as turbid and milky in character with triglyceride levels above 200 mg/dl [1, 8]. In our patient, analysis of the fluid encountered during laparoscopy showed triglyceride levels of 3362 mg/dl, well above the diagnostic marker. Imaging studies, such as CT, lymphoscintigraphy and lymphangiography, also have roles in diagnosing chylous ascites preoperatively [1].
The most important initial step is treatment of the underlying cause of the chyle leak [3, 9]. In this case, reduction of the paraesophageal hernia was imperative to relieve potential compression of the thoracic duct as well as to treat the incarcerated hernia. Medical management is typically aimed at improving nutritional status and decreasing chyle flow, thereby allowing spontaneous closure of the chyle leak [9]. A high-protein and a low-fat diet with middle-chain fatty acids has proved successful [1]. Numerous case reports have endorsed pharmacotherapy such as octreotide and somatostatin either alone or in combination with total parenteral nutrition in managing a refractory chyle leak [1, 2, 9]. In cases of chylothorax, pleuro-peritoneal shunts or chest tubes are found to be useful, especially if severe dyspnea is present [10]. Although there currently lacks a universal approach to treating chylous leakage, surgical reduction of the hernia and dietary restriction were successful in our atypical case.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- cancer
- liver cirrhosis
- deglutition disorders
- diet
- epigastric pain
- chyle
- chylous ascites
- chylothorax
- emergency service, hospital
- hernias
- laparoscopy
- lymph
- operating room
- greater sac of peritoneum
- thoracic duct
- vomiting
- diagnostic imaging
- lipids
- mediastinum
- pleura
- chest
- paraesophageal hernia
- hiatal hernia repair
- compression



