-
PDF
- Split View
-
Views
-
Cite
Cite
Jignesh Tailor, Zane Jaunmuktane, Sebastian Brandner, Huma Sethi, Supratentorial ependymoma presenting as a cortical cyst with a mural nodule in an adult, Journal of Surgical Case Reports, Volume 2015, Issue 1, January 2015, rju124, https://doi.org/10.1093/jscr/rju124
Close - Share Icon Share
Abstract
Supratentorial ependymoma is a rare tumour in the adult central nervous system. We present an unusual case of supratentorial ependymoma in a young adult that presented as a pure cortical cyst with a mural nodule and discuss the differential diagnosis of such lesions in the brain.
INTRODUCTION
Ependymomas are thought to arise from ependymal cells lining the cerebral ventricles and the central canal of the spinal cord. Although they can arise throughout the neuroaxis, they are most commonly found in the posterior fossa in children, and the spinal cord in adults. Supratentorial ependymomas are rare and can appear very similar to other primary central nervous system (CNS) tumours such as oligodendroglioma, central neurocytoma or pilocytic astrocytoma [1]. For these reasons, they are often difficult to diagnose. We present a rare case of supratentorial ependymoma that presented as an isolated cortical cyst with a mural nodule in a 27-year-old woman and discuss the differential diagnosis of cyst with a mural nodule in the brain.
CASE REPORT
A 27-year-old lady presented to the hospital with a single focal seizure. She described flashing lights in her right visual field. Neurological examination was normal and she had no visual field defects or sensory disturbances. Magnetic resonance imaging (MRI) revealed a 2.8 × 2.9 cm lesion in the left parietal lobe, which was predominantly cystic with a murally enhancing nodule (Fig. 1). There was no enhancement of the cyst wall itself. The cyst content was isointense to cerebrospinal fluid (CSF) on T1- and T2-weighted imaging. There was minimal perilesional inflammatory change or mass effect and no restricted diffusion.
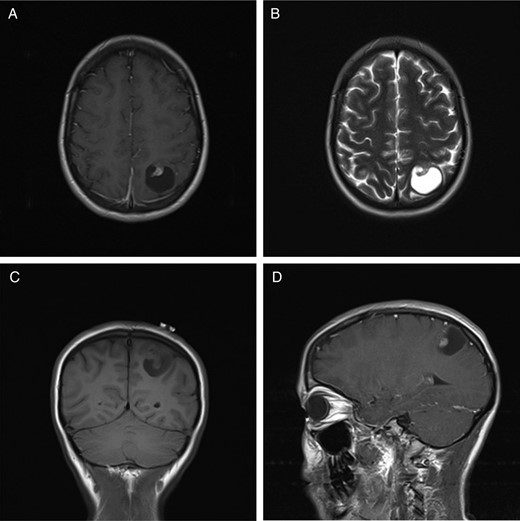
MRI of a supratentorial ependymoma that presents as a single cyst with a contrast-enhancing mural nodule. (A) T1-weighted axial image with contrast. (B) T2-weighted axial image. (C) T1-weighted coronal image without contrast. (D) T1-weighted image in a sagittal plane with contrast.
The possibility of pilocytic astrocytoma was entertained and the patient was offered surgery after discussion in a specialist multidisciplinary team meeting. A left parietal craniotomy and gross total resection of the lesion was performed under image guidance. The tumour had a large cystic component containing straw-coloured, xanthochromic fluid and a solid 1.0 × 1.5 × 2.0 cm nodule. It was well demarcated from the surrounding parenchymal tissue, and there was no communication with the ventricular system. A gross total microscopic resection of the tumour was performed and there were no intraoperative or postoperative complications.
The histopathological examination revealed a moderately cellular tumour comprising variably pleomorphic cells with fibrillary processes and mainly rounded nuclei with a coarsely speckled chromatin pattern. The fibrillary processes of the tumour cells frequently were arranged around the tumoural blood vessels in a radial manner forming perivascular pseudorosettes. In addition, there were large foci of calcifications in the tumoural stroma. No areas showing high cell density, microvascular endothelial proliferation or necrosis were evident and mitotic activity was inconspicuous. Immunostaining for glial fibrillary acid protein (GFAP) showed widespread labelling in the cytoplasm and processes of the tumour cells. Immunostaining for epithelial membrane antigen (EMA) revealed frequent perinuclear dot-like labelling as well as highlighted occasional ependymal canals characteristic of ependymal tumours. Immunostaining for isocitrate dehydrogenease 1 harbouring R132H mutation (IDH1 R132H) was negative. R132H mutation in the IDH1 gene is the most common mutation seen in diffusely infiltrative gliomas such as diffuse astrocytomas and oligodendrogliomas, but not observed in ependymal tumours. The Ki67 proliferation index in the tumour was low (<3%). Overall, the histological features were consistent with a conventional ependymoma (WHO grade II; Fig. 2). The patient was discharged on Day 5 postop and followed up with serial MRI.
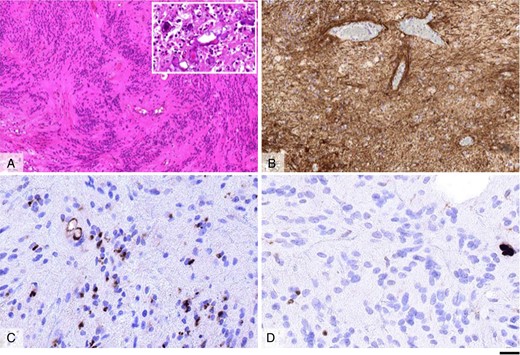
Morphological appearances of the ependymoma, WHO grade II. Haematoxylin and eosin-stained section (A) shows a moderately cellular tumour with frequent perivascular pseudorosettes and areas of stromal microcalcifications (inlet in A). Immunostaining for GFAP reveals widespread labelling in the tumour cells (B); whereas that for EMA shows frequent perinuclear dot-like labelling and accentuates occasional small ependymal canals (C). The Ki67 proliferation index in the tumour is low (D). Scale bar: 100 µm (A and B), 20 µm (C and D), 60 µm (inlet in A).
DISCUSSION
The classic radiological features of a cyst with the mural nodule are usually observed with low-grade pathologies such as ipilocytic astrocytoma (peak age 5–15 years) and haemangioblastoma (peak age 40–60 years). These tumours are most commonly found in the posterior fossa, and the cyst content is usually slightly hyperintense to CSF on T1-weighted imaging [2]. Other tumours with cyst with a mural nodule appearance are pleomorphic xanthoastrocytoma (peak age 10–30 years), ganglioglioma (peak age 10–20 years) and desmoplastic infantile ganglioglioma (peak age 1–2 years). These tumours are usually found in the supratentorial compartment and the cystic portion is hypointense on T1-weighted MRI. Very rarely, metastatic tumours can also present as cyst with a mural nodule [2]. To our knowledge, this is the first reported case of supratentorial ependymoma presenting as a pure cortical cyst with the mural nodule in an adult. Only one previous report of such lesion was found in a 9-year-old boy [3].
Ependymomas represent 4% of all CNS tumours in the adult [1]. They are more common in children, and usually occur in the infratentorial compartment. A review of the literature reveals that supratentorial ependymomas tend to be different from their infratentorial counterparts: First, while the majority of infratentorial tumours are intraventricular, supratentorial ependymomas are usually intraparenchymal. These differences may relate to the developmental origin of these tumours. For example, supratentorial ependymomas may arise from foetal rests of ependymal cells that are located in the angle of the ventricles deep within the cerebral parenchyma [4]. Secondly, a higher proportion of supratentorial ependymomas are high grade (50–60%) compared with infratentorial ependymomas (10–40%) [3]. Thirdly, in gene expression profiling studies, supratentorial tumours cluster separately to posterior fossa and spinal cord tumours, suggesting that they represent a molecularly disparate group of tumours [5].
In conclusion, supratentorial ependymoma is a rare tumour, which can rarely present as a single cortical cyst with a mural nodule on imaging. The possibility of ependymoma should be considered in any case of supratentorial cyst with the mural nodule.
CONFLICT OF INTEREST STATEMENT
None declared.



