-
PDF
- Split View
-
Views
-
Cite
Cite
Yoshiko Uno, Shintaro Nakajima, Fumiaki Yano, Ken Eto, Nobuo Omura, Katsuhiko Yanaga, Mesothelial cyst with endometriosis mimicking a Nuck cyst, Journal of Surgical Case Reports, Volume 2014, Issue 6, June 2014, rju067, https://doi.org/10.1093/jscr/rju067
Close - Share Icon Share
Abstract
We report a case of mesothelial cyst protruding from the right femoral ring with suspected endometriosis in a 35-year-old woman, who complained of a lump with a diameter of 6 cm in the right inguinal region. Although she had the hormone therapy during the next 8 months for the diagnosis of extragenital endometriosis, her symptoms did not improve. The clinical suspicion of a Nuck cyst with endometriosis, supported by ultrasonography and magnetic resonance imaging, was confirmed by histopathological examination of the surgical specimen. Authors herein report this unusual case and review the literature.
INTRODUCTION
Extragenital endometriosis in the inguinal region accounts for 0.8% of the whole endometriosis, which is a common gynecologic condition in the pelvis, which frequently present as a Nuck cyst. We herein report a very rare case of mesothelial cyst protruding from the femoral ring. This case highlights that inguinal mass in women of fertile age is not always a Nuck cyst, and the possibility of other hernia or cyst showed be included in the differential diagnosis.
CASE REPORT
A 35-year-old woman was referred to our hospital for a painful right groin tumor which grew in size which was not related to her menstrual cycle. With the diagnosis of inguinal endometriosis, she had been treated with two cycles of low-dose birth-control pills, and five cycles of genogest previously, but the groin was increased in size to 5-cm with pain. In her past medical history, no history of gynecologic problems and specifically no dysmenorrhea nor dyspareunia were recorded. In the right groin, there was a 5-cm bulge which was detected as a homogeneous hypoechoic subcutaneous tumor and measured 53 × 29 mm by ultrasonography (Fig. 1). Her serum cancer antigen-125 was elevated to 95.4 U/ml (range <35 U/ml) before starting hormone therapy, and down to 40 U/ml when she came to our hospital even though the tumor size was unchanged. Magnetic resonance imaging (MRI) revealed a 6-cm unilocular tumor with internal high intensity in T1WI image which suggested internal bleeding (Fig. 2). We diagnosed the right inguinal tumor as a Nuck cyst. An inguinal approach was selected and after opening the skin and subcutaneous fat, a dark red tumor was founded which protruded from the femoral ring, in spite of our initial impression that the tumor was located along the round ligament (Fig. 3). After careful dissection, the tumor turned to be a unilocular cyst containing serous fluid, which was connected with the peritoneum through a string structure at the femoral ring, which was not connected with the abdominal cavity. The cyst was excised and the string structure was resected at the femoral ring. We inserted a plug into the extended femoral ring, and confirmed no other hernia. Her postoperative course was uneventful, and she was discharged on the first postoperative day. The histopathologic examination showed that mesothelial cells lined the wall of the cyst with degeneration, inflammation, hemorrhage, formation of hyperplastic collagen fiber and hemosiderosis without malignancy (Fig. 4). The immunohistochemistry [Calretinin(+)] confirmed the mesothelial origin of the cyst-lining cells and [CD10(+), ER(+), PgR(+)] suggested the endometrial origin of a few stromal tissue composing the cystic wall. As of 10 months after the operation, no recurrence of hernia or cyst has been encountered.

A 5-cm mass was confirmed over the right inguinal ligament by physical examination.
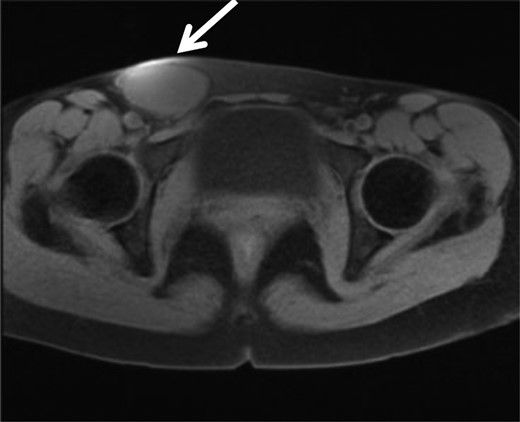
MRI showed a high intensity tumor in T1WI which suggest bleeding in the tumor, in the right inguinal region.
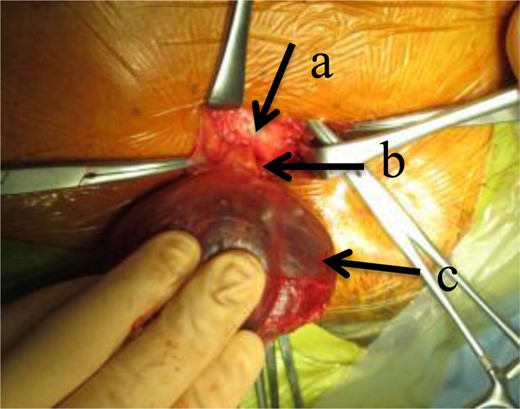
Surgical findings; a dark red tumor was found below the inguinal ligament (arrow a), and a string structure was found through the femoral ring (arrow b), which connected the cyst-like tumor (arrow c) with the peritoneum.
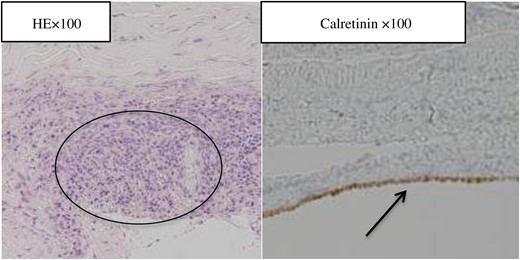
Hematoxylin and eosin-stained section showing a focus of lined mesothelial cells at the wall of the cyst with degeneration, inflammation, hemorrhage, formation of hyperplastic collagen fiber, hemosiderosis and endometrial stroma. The immunohistochemical staining with anti-Calretinin antibody demonstrating positive reaction in the areas where lined cells are of the mesothelial origin.
DISCUSSION
In previous reports, the histological definition of mesothelial cyst, mesothelioma and mesothelial hyperplasia has often been unclear [1]. To our knowledge, there has been only one similar case of mesothelial cyst in which a unilocular cyst protruding from a femoral ring was reported in a 82-year-old female [2]. However, the disposition of mesothelial cells was different from the current case. In the current case, the cyst wall was lined by mesothelial cells, whereas a few mesothelial cells were present at the cystic wall in the other case.
Makunike et al. [3] reported an obstructed femoral hernia with endometriosis in a 43-year-old female, which demonstrated similar clinical pictures; fertile-aged female, right groin mass, mass protruding from the femoral ring and with endometriosis, which was different histologically and embryologically. The current case was diagnosed as endometrial stroma in a mesothelial cyst, whereas their case demonstrated endometrial gland in fibro-adipose tissue and epithelial cells.
Endometrial cyst contained endometrial gland, and the stroma shows the symptom with increased bulk and pain with the menstrual period in 50% of the cases [4, 5], with the right groin predominance [6].
In the current case, the mass did not reduce after hormone therapy and we therefore chose operative treatment. We identified only an endometrial stroma in a part of the cystic wall of the excision specimen, which cannot be diagnosed definitively as endometriosis. However, co-existence of aberrant endometriosis is suspected, and it is possible that preoperative hormone therapy has reduced endometrial gland and stroma to transform femoral hernia into a cyst by interruption of the communication with the peritoneal cavity.
From preoperative physical examination and image views, the mass was identified cephalad to the inguinal ligament and diagnosed as inguinal hernia. Correct diagnosis was made difficult probably because the tumor turned over strand structure.



